Science / Tech
Medications Can Help Keep Alcoholics Sober. Why Are They Being Ignored?
Affordable, safe, generic anticonvulsants restore homeostasis to the brains of chronic drinkers, but they are not being promoted.
Quitting alcohol is easy. People do it all the time. Staying sober long-term, however, is a different story. The average substance abuser quits 5.4 times before achieving prolonged sobriety, and that number is likely much higher among those who never get sober. Eighty-five percent of alcoholics relapse within the first year of abstinence. Forty to 60 percent relapse within a month. Even problem drinkers who receive liver transplants relapse at rates reported as high as nearly 50 percent.
The chronic, relapsing nature of alcohol addiction has baffled the medical world for centuries. Why do well-meaning, motivated patients so often return to an activity they know will likely destroy their health, their sanity, their lives, and the lives of their loved ones?
Science now has an answer. Long-term alcohol abuse causes dysregulation in brain chemistry and neural function that can last for months or even years after the initial period of detoxification. Perfectly sober patients, who are well past the detox phase, often experience crushing levels of anxiety, insomnia, irritability, depression, loss of appetite, and anhedonia (the inability to take pleasure in any aspect of life). Addiction experts now believe these post-withdrawal symptoms are a driving force behind chronic relapsing.
Fortunately, a family of drugs that might loosely be called non-benzodiazepines anticonvulsants (NBACs) often restores homeostasis to the brains of patients suffering from what doctors call “protracted withdrawal syndrome.” Unfortunately, most recovering alcoholics never hear about these medications
An Open Secret
The underutilization of pharmacotherapy in treating alcohol use disorders is pretty much an open secret among certain healthcare providers, mostly addiction therapists, liver specialists, and psychiatrists. A small but growing number are calling for increased prescribing and larger clinical trials. This editorial movingly makes their case.
Medications that fall into the NBACs category were developed in the 20th century to treat seizures, convulsions, and/or epilepsy. They include baclofen, carbamazepine, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide. The three that have received the most study and use for post-withdrawal symptoms are baclofen, gabapentin and topiramate. From the outset, researchers noted that, in addition to anticonvulsant benefits, these drugs induced mood stabilization. A 1976 study mentioned in passing that baclofen might be effective at treating alcoholism.
Currently, only a tiny fraction—around one percent—of alcoholic patients ever receive these drugs, despite multiple investigations showing NBACs prolong sobriety and two medical associations advocating their use in their clinical practice guidelines. With at least 14 million people suffering from alcohol-use disorders in the US alone, the global population who could benefit from NBACs easily runs to the millions, if not tens of millions.
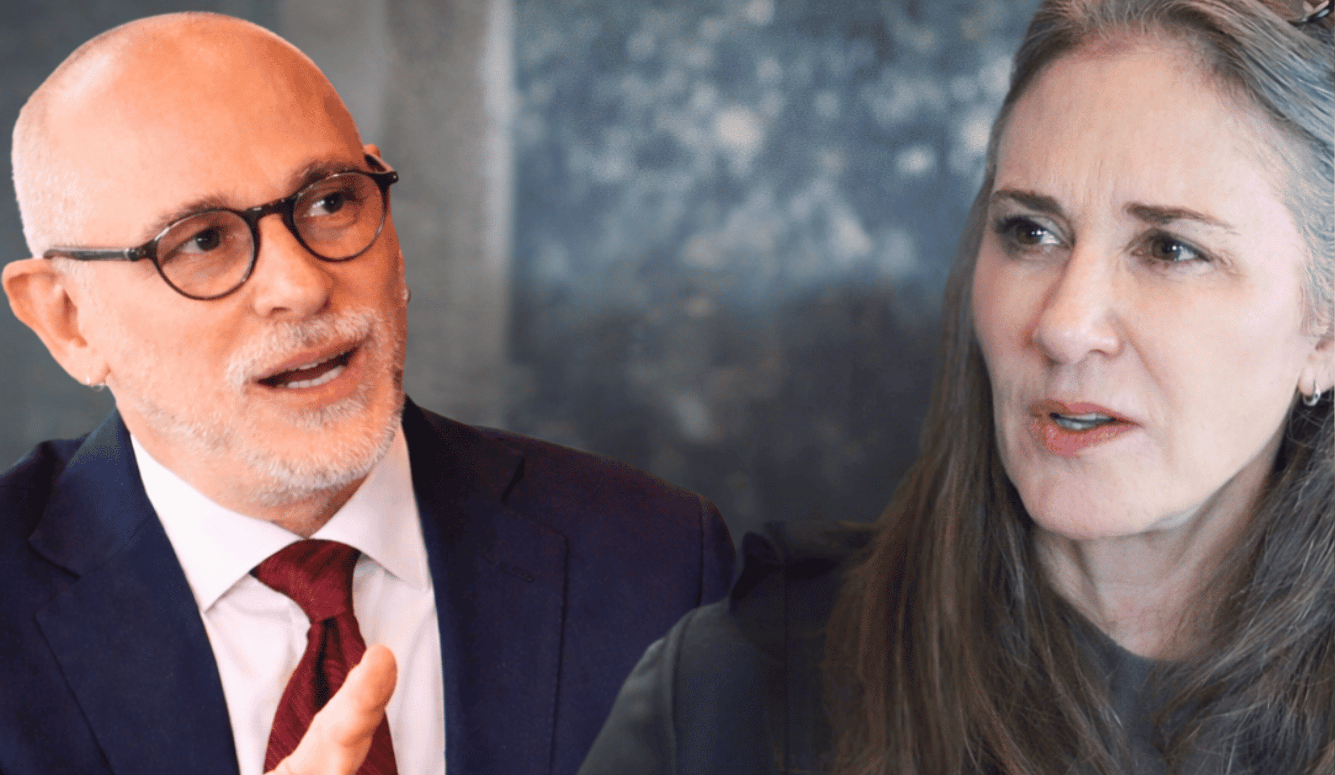
Why are so few patients receiving evidence-based care? One major reason is clearly economic. When a drug’s patent expires, it becomes generic, meaning any pharmaceutical company can sell it. This competition causes its price to plummet. “If something is generic, why would any one company pick up the tab for its marketing?” notes Barbara Mason, PhD, director of the Pearson Center for Alcoholism and Addiction Research at Scripps Research in San Diego, CA.
Without the gargantuan profits that flow from exclusive rights to sell a drug, the large pharmaceutical companies simply aren’t interested, she explains. “I would say that scientists have been working hard to bring these potential medications forward,” she added, “but it really takes a big pharmaceutical company to do the kind of marketing that penetrates the awareness of potential prescribers and patients. So, yeah, that’s a difficult thing.”
How NBACs Work
To understand how NBACs work, we need to look at the neurochemistry behind protracted withdrawal syndrome, also known as protracted abstinence syndrome or post-acute withdrawal syndrome (PAWS).
Drinking enhances the release of the neurotransmitter gamma-aminobutyric acid (GABA), leading to a pleasurable feeling of relaxation. Prolonged alcohol use causes the brain to counteract higher GABA levels by producing less of it. The alcohol-soaked brain also increases production of glutamate, a stimulant. When drinking abruptly stops, the brain experiences an imbalance in these neurotransmitters: too much glutamate, too little GABA. This creates the classic withdrawal symptoms of anxiety, irritability, sleeplessness, tremors, seizures, etc., which last about three days to seven days.
After acute withdrawal passes, brain chemistry returns to normal, and symptoms subside. However, among some patients with a prolonged history of drinking—on a timescale usually measured in decades, so the condition often strikes middle-aged and geriatric subjects—something starts to occur around the one- to three-month mark of abstinence.
The classic withdrawal symptoms begin to return, mild at first but slowly progressing in severity. Researchers were initially mystified by this phenomenon. To the eyes of science, these patients were completely “clean,” their blood plasma free of the biomarkers and toxic elements that characterize alcohol addiction. Why were they re-experiencing the hallmark symptoms of alcohol withdrawal several months after detox? Most scientists put it down to a psychological problem, or even just addictive personalities fabricating complaints to conceal a lack of willpower.
But further investigation revealed that while blood chemistry among PAWS patients was healthy, their brain chemistry was not. Both animal and human subjects show persistent regional glucocorticoid dysregulation that leads to alterations in the hypothalamic-pituitary-adrenal axis, a known prime driver of alcohol addiction.
In the past, many PAWS patients were given openended benzodiazepine prescriptions. Benzodiazepines (drugs like Xanax, Klonopin, Valium, etc.) certainly do relieve symptoms, but in the end, they merely swap one addiction for another. “I commonly tell my patients, if I’m giving you a benzo, I’m just giving you alcohol in a pill form,” says Anil Bachu, MD, a psychiatrist who directs an in-patient medical center in Little Rock, AR where he occasionally prescribes NBACs.
Unlike benzodiazepines, NBACs have a low addiction profile, according to Dr. Bachu. They are non-euphoric, meaning patients don’t feel “high” while on them. Patients also don’t build up a tolerance to these drugs. That is, it doesn’t take larger and larger doses to achieve the same effect. When they work, NBACs simply relieve symptoms and make patients feel normal. Sleep, appetite, mood—all return to normal. The only difference is patients often attain a complete indifference to alcohol, leading to long-term sobriety without effort.
Science is not completely sure how NBACs alleviate symptoms while avoiding the pitfalls of addiction, tolerance, and intoxication, but it’s theorized that they impact brain chemistry in uniquely subtle ways. For example, benzodiazepines target GABA type A receptors, which produce a quick and pleasurable surge of dopamine to the brain. This receptor plays a central role in dangerously addictive drugs like heroin. NBACs, on the other hand, tend to target GABA type B receptors, which produce slower, more prolonged inhibitory signals. Some NBACs sidestep GABA receptors altogether, acting instead on voltage-gated calcium or sodium channels.
To be clear, these drugs are not perfect. They don’t work on every patient. They have side effects, as all medications do. And although NBACs are not addictive like opioids or benzodiazepines, if treatment ends too soon, symptoms may return. So, in that sense, patients are physically dependent on them. The catch here is no one knows for certain how long treatment should last. At least not yet. It’s probably different for each NBAC. Notably, however, a French doctor who’s managed more than 1,000 baclofen patients found treatment could be discontinued after “one or a few years.”
Barriers to Acceptance
In fairness, lack of profitability is not the only reason NBACs are being largely ignored. For starters, addiction therapy has a long history of hyping pharmacotherapy cures that fail to deliver.
Many physicians alive today remember the mass prescribing of benzodiazepines that ended in disastrous double addictions. In 2006, a medication called Prometa, a cocktail of three widely available drugs said to induce abstinence after a single one-month treatment, proved ineffective. Then there was ibogaine, a psychedelic popular in the 1980s that not only yielded questionable results but also caused the deaths of over a dozen patients. This checkered history may be contributing to a wait-and-see approach.
Another barrier is that, while NBACs are FDA-approved as anticonvulsants, they’re not specifically approved for alcohol use disorders. Which means that, in this context, they’re “off-label” medications. Off-label prescribing is a perfectly normal and accepted practice in healthcare, but it still can make physicians uneasy. Dr. Bachu himself admits he’d like to see larger peer-reviewed studies before prescribing these drugs more frequently.
However, there already are three FDA-approved medications for alcoholism: disulfiram, naltrexone, and acamprosate. While probably not as effective at maintaining long-term abstinence as NBACs, they still provide benefits—yet they too are grossly underutilized.
Much of the problem boils down to lack of awareness among practitioners, according to Dr. Mason. Gabapentin is known to many, she says, but the other NBACs remain mostly the domain of substance abuse specialists, usually psychiatrists. “We have a lot of good science around potential pharmacological treatments for alcohol use disorders,” she concludes. “We just have to get the word out to the public.”