Patient Safety and the Medical Omerta
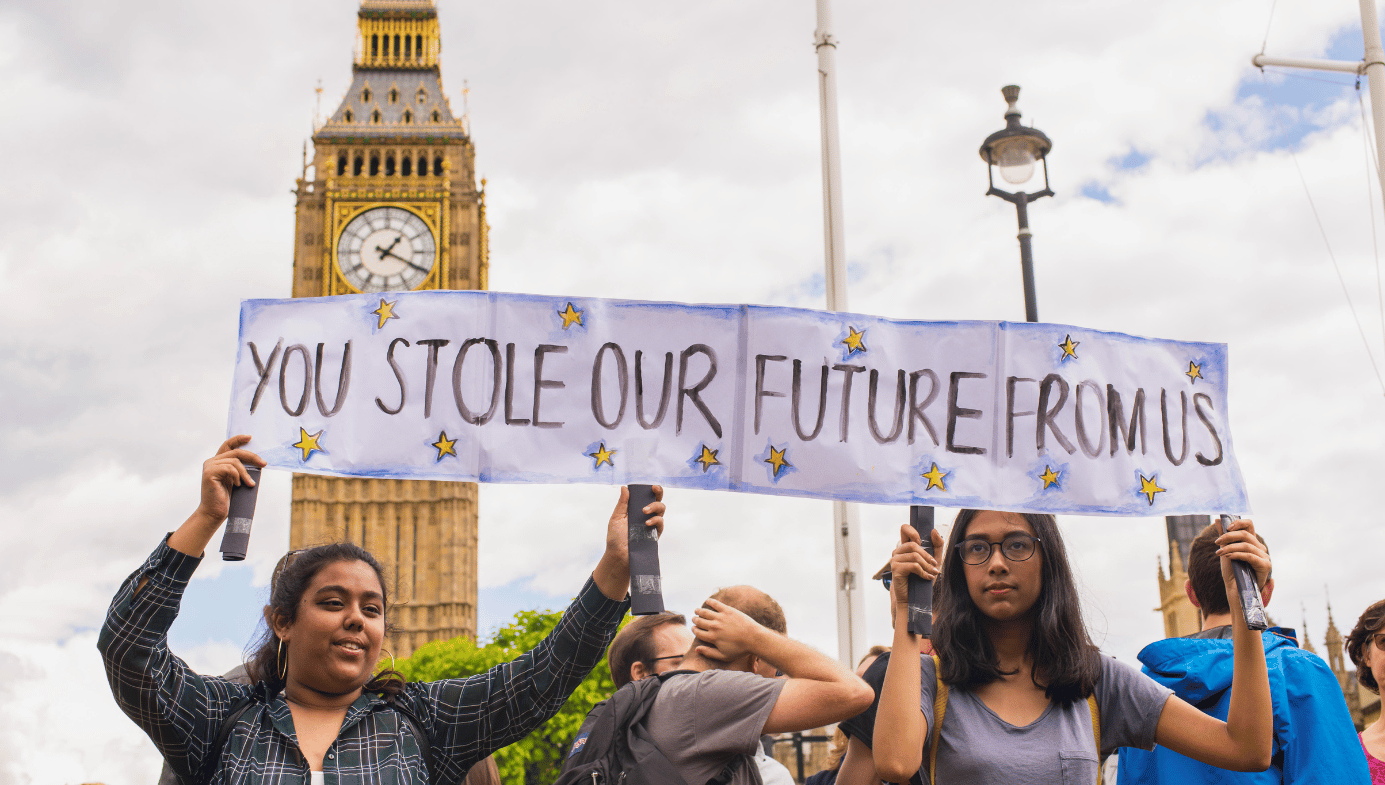
The sharp decline in popularity of the Catholic Church shows how difficult it is for public trust to be regained once power is abused—if the medical profession does not take its responsibility to protect patients more seriously it risks losing this trust.

September 17th, 2020 will mark the second anniversary of the World Health Organisation’s World Patient Safety Day, a sign of the progress made in highlighting the risks of iatrogenesis—harm caused by medical negligence or error. The loosely defined patient safety movement grew from the work of the American paediatric surgeon Lucian Leape, and the publication of the 1999 Institute of Medicine paper ‘To Err is Human,’ both of which succeeded in drawing attention to the risk of being inadvertently killed or otherwise mistreated by healthcare providers. The patient safety movement has subsequently called for better detection and investigation of error, and while official UK data estimates up to 12,000 deaths from medical error per year, the voice of the medical profession in these matters has been conspicuously quiet.
Inquiryitis
Here in the UK, there has been no shortage of healthcare scandals within the publicly funded National Health Service (NHS). The history of public inquiries into the NHS reminds us of the inherent power imbalance between healthcare providers and the public. However, over 130 such inquiries have been held since the NHS’s founding in 1948, so the announcement of yet another has long since ceased to be a notable event. The number of recommendations in these reports has so far ranged from 0 to 290, but an invariable feature is the refrain that learning from previous inquiries failed to take place. Following the bizarre occurrences at Ashworth Hospital in the 1990s, the Fallon Report coined the term “Inquiryitis” to describe the reflexive launching of inquiries following any major healthcare scandal.
Inquiries may be useful for establishing the facts of what occurred (although even this has been disputed),1 but what use does this serve if lessons are not learned? And whose job is it to enact the recommendations anyway? Sara Ryan of Oxford University writes that the cathartic release that public inquiries allegedly provide to affected families sidelines the pain and labour that bereaved families endure before, during, and after the investigative process.2 In Ryan’s case, the healthcare provider denied accountability for the death of her 18-year-old son Connor Sparrowhawk for almost five years; in her words, “Families should not have to fight for justice and accountability from the NHS.” But since this remains the case, it is unclear what the inquiries have achieved besides a demonstration of performative scrutiny.
The risks of self-regulation
There has certainly been some progress in levelling the playing field for the public’s dealings with doctors. A relative increase in democratic participation, increased suspicion of traditional institutions, and easier access to information have resulted in a medical profession that is more inclined to respect the rights and rational capabilities of patients than in previous centuries.
But the power of the medical profession is not just limited to the intimate interaction between doctor and patient. The training the profession receives, along with the specialised language and its associated rarefied meanings, allow for a patient’s treatment to be recorded in a manner that is almost unintelligible to anyone but other medical practitioners, and often further limited to those within the same specialty. A gynaecologist’s decisions, for example, are difficult to judge unless by another gynaecologist, or perhaps an experienced specialist nurse in gynaecology.
This allows for the development of a form of tribalism that protects against internal scrutiny and can allow entire departments, even entire medical specialties, to engage in practices that would be considered unethical to the outside world but, given how widespread they are, are then described as “cultural.” But not all unethical behaviour is embedded within, and therefore blameable upon, a culture. Sometimes inaction from the medical profession after patients are harmed is the result of a rational and self-interested decision.
The medical profession’s inaction
Even a cursory examination of public inquiries and high-profile medicolegal cases reveals how often doctors have been aware that harm was being inflicted on patients but took little or no action to expose it. Other staff, such as nurses, physiotherapists, and administrators may have been aware. Nevertheless, doctors are best placed to decipher the obfuscatory language used to smokescreen questionable practices, and along with their higher incomes, they enjoy a more privileged social standing and have a codified duty to speak up courtesy of the General Medical Council (GMC).
The profession’s track record on speaking up is poor, even so. The British serial killer Harold Shipman was generally respected by his medical colleagues until Linda Reynolds, a GP who had been working in the local area for just a few months, pursued an investigation into his murders. The anaesthetist Stephen Bolsin was singular in raising concerns about the high death rates within the Bristol paediatric cardiothoracic department and paid the price by being unable to find employment in the UK after those concerns were vindicated. The Mid-Staffordshire Inquiry Report exposed poor nursing and medical care that caused several hundred deaths—it makes for depressing reading, not least because so few medical staff raised the alarm. One such death was that of Gillian Astbury, a 66-year-old diabetic lady who died after a 10-day admission with hyperglycaemia due to insufficient insulin. A nurse lost her licence to practise due to a failure to check and administer Gillian’s glucose control. Yet, even though no medical notes were recorded on several days and there was no evidence that the fatal diagnosis was considered prior to her death, no doctor was held similarly accountable.
Although poor clinical care may indeed result from a normalisation of low standards due to poor leadership and chronic underfunding, this does not justify inaction when doctors become aware of a problem. Doctors report that a major barrier to speaking up is a fear of reprisal but this explanation is unsatisfactory given that concerns can be raised anonymously. A GMC survey of doctors in 2013 found that just five percent of respondents had unaddressed concerns about patient care in the past year. Of these, around a third had never reported their concerns before completing the survey.
Counterintuitively, as doctors became more experienced the chance of them having concerns about patient safety actually fell, with just 2.8 percent of the most experienced doctors in the survey having any concerns. It is also worth noting that 83.5 percent of respondents had no concerns at all about patient care in the past year, compared to the 77 percent of nurses who believed that patient care was compromised “several times a month or more” due to short staffing. Notwithstanding this dubious lack of awareness, a valuable 2018 survey by Archer and Colhoun revealed that even when consultants were aware of patient safety incidents, the majority of concerns were simply not reported.3
Who are the second victims?
When professor Sir Liam Donaldson, former NHS Chief Medical Officer and former WHO Envoy for Patient Safety delivered the Parliamentary and Health Service Ombudsman Annual Lecture in 2018, he remarked that, “The patient safety literature talks about the second victim. Our principle concern is, of course, for the patient that’s harmed, but there is also harm for the staff involved.” An entire academic literature exists describing the suffering of these “second victims”—there is even a taxpayer-funded website offering resources to support staff traumatised by the harm inflicted on the patient. Bereaved families, meanwhile, have to rely on Action against Medical Accidents, Inquest, and other such charities, and fundraising efforts to cover the costs of legal counsel.
On December 23rd, 2010, a previously healthy three-year-old boy named Sam Morrish died of sepsis. Despite years of denial from the hospital’s staff, it was eventually revealed that errors at every level of NHS care had been made and his death was entirely avoidable. The consultant paediatrician, a former medical director at the hospital, did not look at the notes before signing the death certificate and therefore claimed to be unaware of the major delay in antibiotic administration that contributed to Sam’s death. Although Sam had been under his care, he later chaired the “impartial” meeting to review the child’s clinical management. Unsurprisingly, the outcome of this and the hospital’s subsequent internal review was that the death was tragic but unavoidable. It was only after four years of persistence from the family that the litany of errors came to light.
Harry Richford’s birth and death just seven days later was so poorly managed that the events would be more typical of Third World healthcare. The hospital and its doctors denied error for as long as possible, and even claimed on the Child Death Notification Form that the death had been “expected.” It took two years for the hospital and its staff to accept responsibility, but only after an official inquest report was published—an inquest which had to be instigated by the family because the hospital’s staff refused to report the case to the coroner.

The experiences of Sam’s, Harry’s, and Connor’s families are unfortunately not rare. Common themes are easy to identify—years of denial, admission of errors but none that materially altered the outcome, highly incompetent and insensitive NHS staff, and a lack of emotional support for the families involved. The case of Bethany Bowen, a five-year-old girl who died from complications of an elective splenectomy, offers a valuable insight into how denial and minimisation of error has become so pervasive. In a memorandum submitted to the Parliamentary Health Select Committee in 2008, Bethany’s mother Clare Bowen wrote this:
The time has to come to acknowledge that medical staff may not always be forthcoming with all the facts following the death of a patient that they were directly involved with. To do so could damage or even terminate their career, and implicate colleagues with whom they work closely.
It should also be recognised that it is not in the interests of the NHS Trust to publish information that reveals human error and serious shortcomings in procedure. They have a reputation to protect.
This may seem obvious, but the experience of the witness both in the 16 months prior to the inquest and during the inquest itself, is that the testimony of the doctors is ultimately decisive in determining the facts.
This echoes Mulcahy’s important 2003 study of NHS complaints which found that “doctors seek to externalise blame, maintain the image of the competent expert-knowledge worker and feel justified in making assertions about the superiority of their form of narrative.”4 The tremendous patience and resilience required by grieving families to question healthcare providers is described by Scott Morrish, Sam’s father, in a statement given to the Public Administration Select Committee in 2015:
The absence of a “system for learning” can force patients into the often dysfunctional and ram-shackle world of complaints systems which in turn, can cause yet more harm. The need for a complaint in such circumstances is, in itself, symptomatic of problems. The burden of learning should not fall upon the shoulders of patients, or depend upon them for impetus, especially at times when most in need of support and least able to cope… Learning should take place irrespective of whether there is a complaint or not.
It is regrettable that, in the academic world, Sara Ryan is unusual in describing the suffering inflicted on families by healthcare providers’ denial and minimisation of concerns. An excellent 2019 BMJ article written by several American patient safety advocates calling for the end of the term “second victims” signals progress in shifting the focus from the perceived needs of healthcare staff towards greater justice for patients and their families.5 Considering the term populated the literature for almost two decades with little dissent from the Academy testifies to the difficulty of the task that patient safety advocates have taken on.
The limitations of the “human factors” literature
While doctors fail to speak up in the face of avoidable harm, the academic specialty of “human factors” provides a space into which discussion of medical error can be funnelled without paying attention to uncomfortable truths. Wachter and Gupta’s Understanding Patient Safety defines human factors as “concerned with the interplay between humans, machines, and their work environments,” providing almost limitless bounds to a conception of medical error which downplays doctors’ responsibilities. References in the human factors literature to the aviation industry’s blame-free reporting culture are common, but the key difference between the two industries is that while an entire airline’s crew has a stake in reporting safety incidents, healthcare staff suffer no ill-effects if harm to patients remains unreported.
The human factors literature construes healthcare workers as lacking in individual agency and only acting in response to some systemic malady, for which policies, protocols, training exercises, or managerial expertise are the prescribed treatment. The downstream orthodoxy is that most clinical errors occur as a result of systemic failings. But is this a tenable position when most clinical errors are never reported? Archer and Colhoun’s study respondents were mostly consultants, and the most common reason for not reporting patient safety incidents was a perceived lack of time. Could it be that incidents related to individual failings are in fact less likely to be reported to avoid criticising oneself or close colleagues?
Unexamined assumptions abound in the patient safety literature and successfully deflect attention from severe flaws in the medical profession that only honest reflection can correct. Soon-to-be-published data show that the rate of reporting of any harmful patient safety incidents by consultants averaged approximately six reports per 100 consultants per year. In light of these data, the idea that doctors are aware of concerns relating to patient care but are doing little or nothing to address them is unsurprising. There is no doubt that the NHS clinical governance systems are weak, but without at least minimal engagement from doctors improvements cannot be expected.
The moral responsibility to speak up
A community’s silence permits moral transgressions. Whether the context is policing or the Hollywood film industry, the public should not accept that unethical and even criminal activity will remain unreported to protect the career interests of those in the know. Even though the medical profession has an unequivocal responsibility to protect patients enshrined in its ethical code, a Freedom of Information request reveals that no doctor has ever been sanctioned for failing to speak up. The GMC would do well to take this responsibility more seriously—it has certainly sanctioned doctors for less important issues.
The sharp decline in popularity of the Catholic Church shows how difficult it is for public trust to be regained once power is abused—if the medical profession does not take its responsibility to protect patients more seriously it risks losing this trust. The paucity of criticism directed at the profession despite the catalogue of NHS care scandals is a source of wonder given the clear abdication of the responsibility to speak up. It is not possible to manufacture a healthcare system based on moral principles unless it is comprised of morally committed agents, and while the rhetoric of putting patients first is apt, the time for action to match it is overdue.
Correction: An earlier version of this article misidentified Linda Reynolds as Sally Reynolds. Apologies for the error.
References:
1 Walshe, K. (2019), Public Inquiry Methods, Processes and Outputs: an Epistemological Critique. The Political Quarterly, 90: 210-215. doi:10.1111/1467-923X.12691
2 Ryan, S. (2019), NHS Inquiries and Investigations; an Exemplar in Peculiarity and Assumption. The Political Quarterly, 90: 224-228. doi:10.1111/1467-923X.12703
3 Archer G and Colhoun A (2018). Incident reporting behaviours following the Francis report: A cross-sectional survey. Journal of Evaluation in Clinical Practice, 24(2). Pages 362-368.
4 Mulcahy L (2003) Disputing Doctors. Open University Press. Page 147.
5 Clarkson MD et al. (2019). Abandon the term “second victim” BMJ; 364 :l1233 doi: https://doi.org/10.1136/bmj.l1233