COVID-19 Updates
COVID-19 Science Update for March 29th: Keep Your Voice Down
The latest research on COVID-19 tells us that “the major transmission mechanisms are not fine aerosols but large droplets.”
This article constitutes the March 29th, 2020 entry in the daily Quillette series COVID-19 UPDATES. Please report needed corrections or suggestions to [email protected].
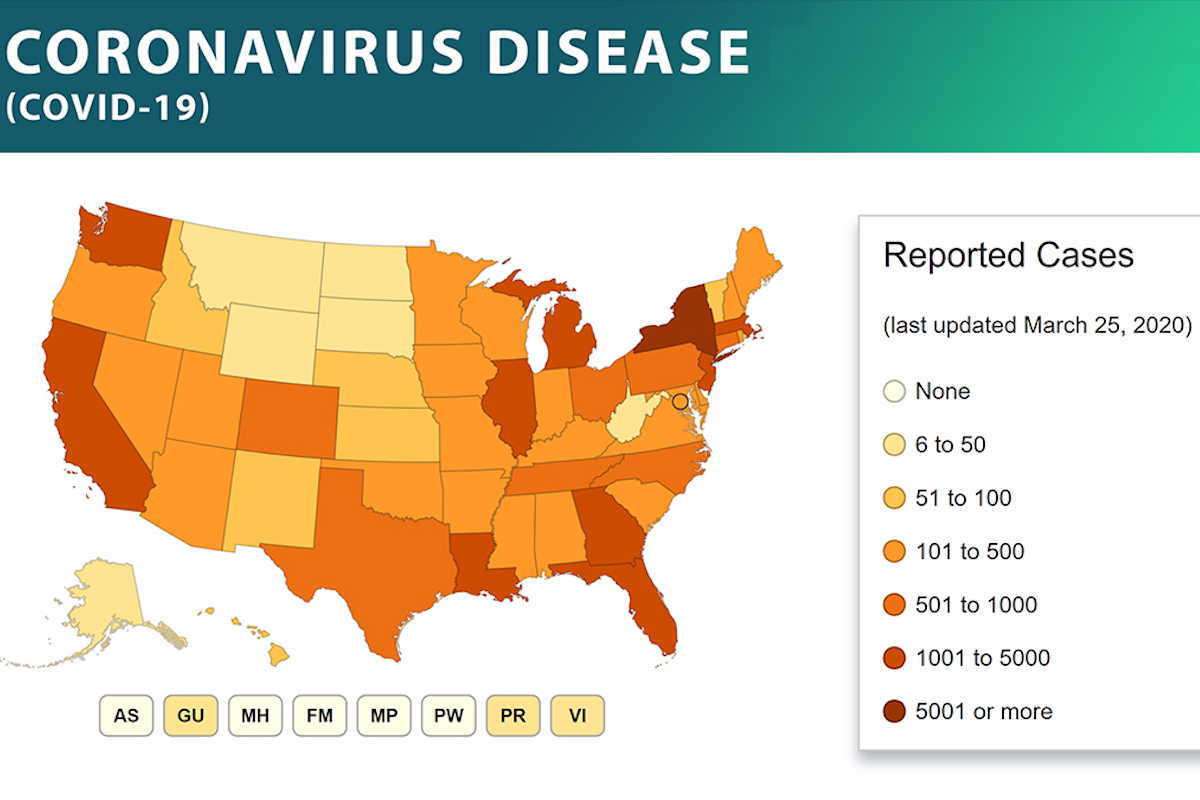
According to statistics compiled by Our World in Data (OWD), the number of newly confirmed COVID-19 deaths increased yesterday. The data, as originally assembled by the European Centre for Disease Prevention and Control (ECDC), indicated 3,461 new confirmed COVID-19 fatalities globally, up slightly from Saturday’s newly reported deaths (3,318). As has been the case throughout mid- and late March, the new deaths were concentrated largely in Italy (887), Spain (832), the United States (411), and France (299). Taken together, these four countries accounted for about 70 percent of all newly reported global deaths—about average for the past three weeks.
In the United States, about half of all cases are located in and around New York. As the New York Times reports, the city’s emergency-response services are becoming overwhelmed, and health care workers are beginning to be faced with the sort of live-or-die decisions that Italian doctors have been required to make. As discussed below, France has substantially addressed the problem of regional case-load concentration with an innovative national-level plan. Unfortunately, this sort of planning seems to lie completely beyond the organizational competency of the US system, and basic policy determinations are being made on the basis of public political posturing.