Vaccines
Will the New Vaccine Help Eradicate Malaria?
The malaria vaccine may well help reduce deaths, but we should not exaggerate its efficacy.
· 7 min read

Keep reading
A Tariff Time-Bomb
Phillip W. Magness
· 9 min read
The Teaching Problem
John Tagg
· 17 min read
Invisible Disability and Hidden Potential
Hannah Gal
· 16 min read
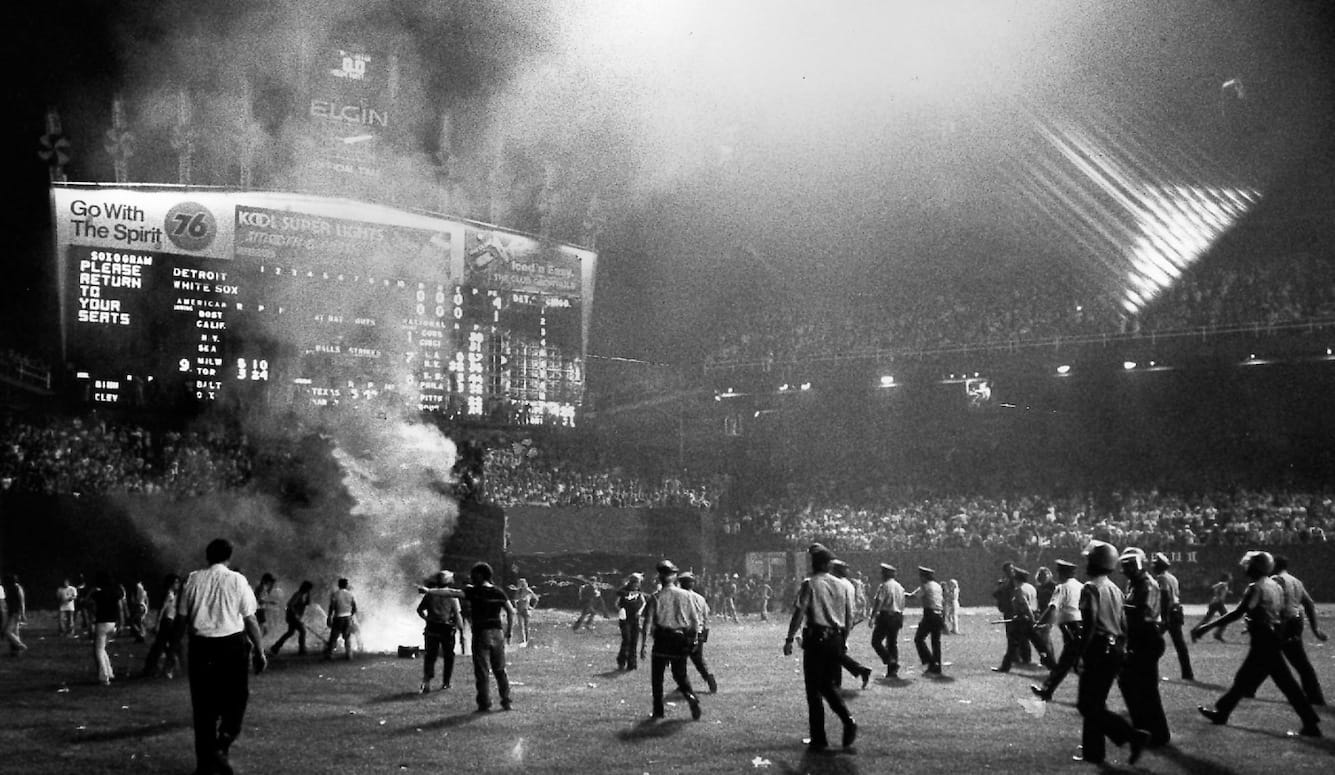
Disco Inferno
George Case
· 10 min read
Conflicting Visions of Peace
Benny Morris
· 8 min read