Science / Tech
Science by Quota
Australia’s unnecessary new NHMRC policy will lead to a decline in scientific quality.

The National Health and Medical Research Council (NHMRC) is an Australian government agency responsible for the country’s largest source of funding for health and medical research. Its funding schemes are highly competitive, and only a small percentage of high-quality projects end up receiving support. This commitment to quality is specified in the organization’s Corporate Plan, which states that it will invest in “the highest-quality health and medical research and the best researchers.”
However, in recent years, its CEO Anne Kelso has committed the organization to prioritising gender equity when awarding grants. Under this policy, the NHMRC has adjusted success rates in various schemes to increase the number of female grant holders. The justification for the gender-equity policy is that females have been historically under-represented among the successful applicants in certain grant schemes. NHMRC has attributed such inequities to “the systemic disadvantage experienced by women in the workforce.” Recently, it announced further efforts to promote gender equity, by awarding equal numbers of grants at the most senior level of its Investigator Grant scheme, which provides generous funding for a productive researcher’s program of work over five years.
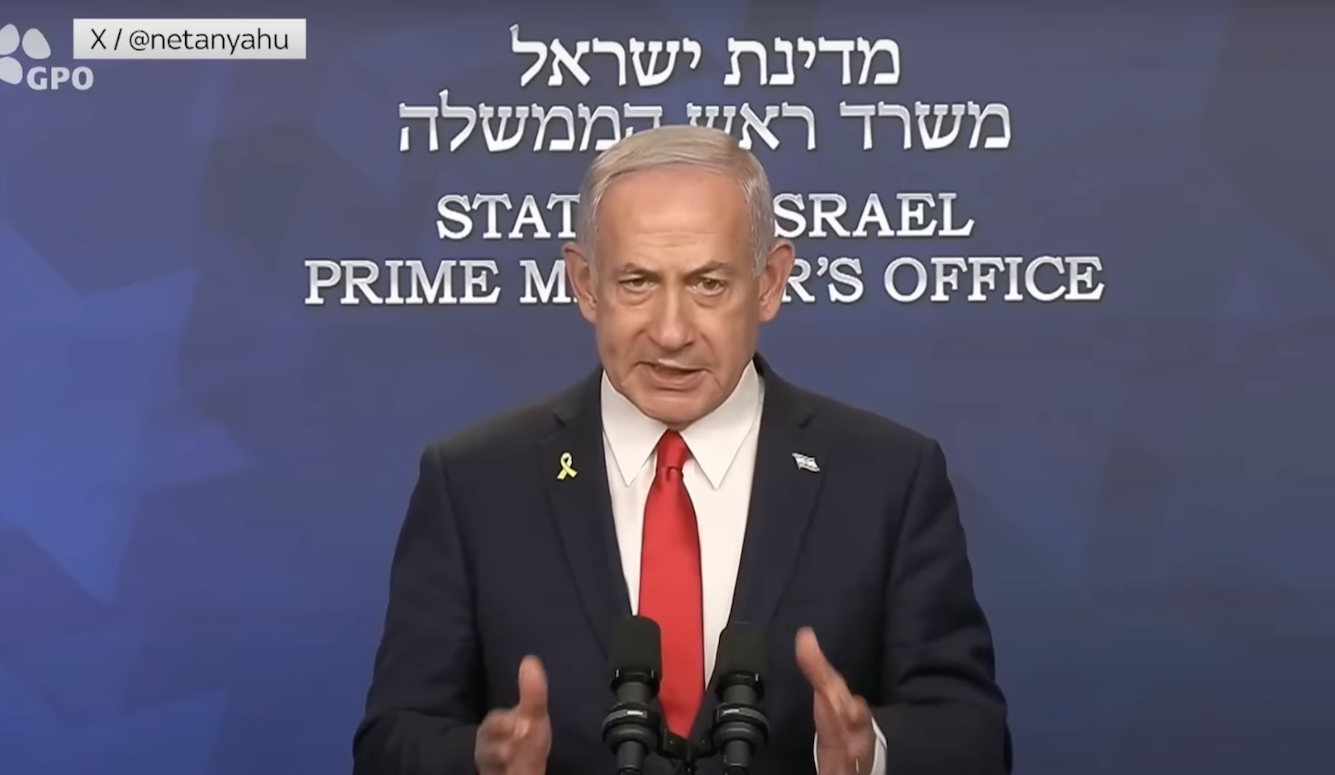
In an essay for Quillette, Lawrence Krauss described the NHMRC approach as “anti-male bias.” He argued that research funds should be allocated on the basis of quality rather than gender or other personal attributes. I agree with Krauss’s conclusion that quality should be the only relevant criterion when considering an application, but I would like to add some personal observations as someone who has been both a recipient of NHMRC funding for many years and a participant in various grant committees and peer-review panels.
I am a senior male researcher in the area of mental health, who has benefited greatly from NHMRC funding. I was fortunate to receive NHMRC salary support from the mid-1980s until 2018. This was by no means easy. Every four years I had to apply in open competition along with anyone else who aspired to obtain salary funding from NHMRC. Given the low success rates, I must have been a very good applicant, but I was also lucky given the uncertainties of peer review. When my children were young, I worried about the need to provide an income with which to support them, and so I always made back-up plans in case I missed out in a funding round, which would have been the end of my career as a full-time researcher.
Along the way, I saw many other researchers who either failed to get re-funded or never managed to enter the scheme at all. The problem is that there has never been enough funding to cover more than a minority of the applicants and projects, so many researchers are frustrated by repeated failure. The minority who are fortunate enough to get funded live with the uncertainty and worry about whether their funding will continue, both for their own salaries as well as for the junior staff who are employed on their grants. One such researcher has recently described health and medical research in Australia as a “high-status gig economy.”
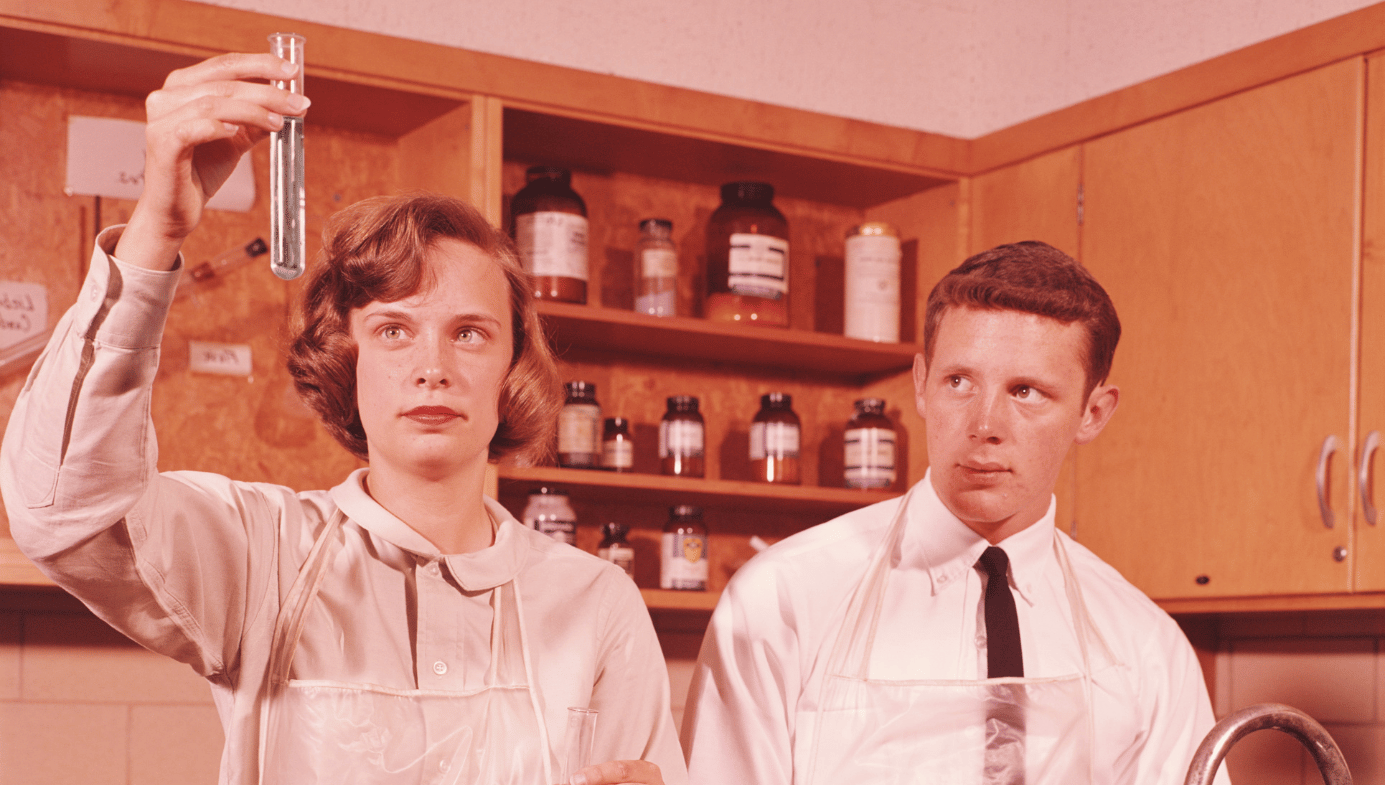
I have also had the experience of sitting on NHMRC grant peer-review panels and on many NHMRC committees, including its top Research Committee, which allowed me to see the other side of the funding schemes. While the peer-review processes have never been perfect, I have always found them to be fair and motivated by the importance of choosing the highest quality projects for funding. The new policy championed by the current CEO means that gender equity will override quality. Any adjustment of grant outcomes by gender necessarily requires that some women with lower quality applications will be favored over some men with higher ones.
In spite of its shortcomings, peer review of grant applications remains the best predictor we have of the quality of future research. Follow-up of over 130,000 research grants funded by the US National Institutes of Health found that peer-review rating consistently predicted later success, with higher rated grants resulting in more citations, publications, high-impact publications, and patents. Evidence on Australian peer-review ratings of grant applications has found no gender difference in quality ratings of research proposals across a wide range of disciplines. Given the lack of gender difference in quality, there should be equal success rates between women and men. Any attempt to increase female success rates artificially to ensure gender parity in grants or funding awarded will undermine the predictive power of peer review and lead to an overall reduction in quality.
The same day the new gender equity intervention was announced, NHMRC also released data on outcomes from grants awarded during 2022. Summed across all schemes, females put in 863 applications as the first-named Chief Investigator, 166 of which were funded (a 19.2 percent success rate) and $263,951,809 was awarded. By comparison, males put in 999 applications, 138 of which were funded (a 13.8 percent success rate) and $254,342,109 was awarded.
These figures provide no indication that female researchers are systemically disadvantaged. However, the recently announced gender-equity policy centers around the most senior level of the prestigious Investigator Grant scheme, which is awarded at five levels ranging from post-docs to very senior researchers. In 2022, females did better than males at the first four levels—in terms of number of grants, success rates, and amounts awarded—but males dominated the most senior level. But as Lawrence Krauss pointed out, the major source of this discrepancy is that many fewer women applied at the most senior level. In 2022, 36 females applied and 15 were successful (a 41.7 percent success rate) compared to 113 males, 26 of whom were successful (a 23 percent success rate).
NHMRC documents have attributed gender differences in applicants at the most senior levels to “attrition,” meaning that fewer women apply because they have dropped out of the system earlier in their careers. However, NHMRC has never produced any evidence to support the attrition hypothesis other than a snapshot of the current distribution of applicants. To show that there has been attrition requires that a group of researchers are followed across their careers and that women drop out over time. Such a study has not been conducted.
Another more plausible explanation is that there has been a generational shift in female participation in higher education and research. To someone my age, this is obvious. In the 1980s, men clearly outnumbered women at conferences and in research meetings. I often attended project meetings where there was only one woman present. Today, it is exactly the opposite. I often attend meetings where I am the only man among a group of much younger women. In Australia, women have been steadily increasing as a percentage of PhDs since the 1950s and achieved parity with males around 2009. Today, females have greater achievement at postgraduate education than males. According to the 2021 Australian census, 56.6 percent of people aged 25–34 years who hold a postgraduate degree are female.
This generational difference is also seen in NHMRC funding applications. In the 1990s, females made up 28.5 percent of applicants for research fellowships compared to 35.6 percent today. This suggests that, in time, females will make up the majority of health and medical researchers at all levels, as older males retire or die and are replaced by younger females.
How long will this gender transition take? I estimated this by looking at the careers of the successful applicants in the most senior level of the Investigator Grant scheme. Using available data, I found that their median year of first career publication was 1991. This implies that it takes over 30 years on average for a researcher to go from first publication to the stage where they could compete successfully for the most senior NHMRC grants. If females reached parity with males in PhD completion in 2009, then I would estimate that parity at the most senior levels will be achieved around three decades after that.
Some might argue that discriminating in favor of senior female grant applicants to compensate for the past low participation of women in higher degrees is morally justifiable. And there may indeed be women who lacked opportunities for a research career in the past. They might have conceivably aspired to a research career but were prevented from doing so by a myriad of factors, such as marriage and children, a greater load of domestic duties, lack of encouragement from elders, not being able to afford the costs of higher education, or a lack of female role models. Unfortunately, positive discrimination towards senior women now, who have been very successful in research and may not have had these disadvantages, does nothing to help those women who missed out in the past.
Furthermore, once the principle is established that outcomes must mirror the distribution of various attributes in the population, then a wide range of similar claims for adjustments could arise, all of which may then be used to override assessments of quality. A similar argument for adjustments could be made on the basis of characteristics such as early-life socioeconomic disadvantage, non-English-speaking background, disability, or belonging to professions that have been traditionally under-represented in research such as social work and nursing.
The younger generation of researchers, both female and male, find it even tougher to get funding than my generation. Success rates in grant applications have been declining for decades. For example, with NHMRC research fellowship funding, success rates in the 1990s were 36 percent for females and 34 percent for males, compared to 21 percent for females and 14 percent for males today.
Even though the funding available for research has increased over time, the number of young people wanting to be researchers has increased even faster. The deep levels of frustration and disappointment in the talented young researchers who miss out are readily apparent to anyone in the industry.
Given that these young researchers are the future of health and medical research, I would rather see NHMRC prioritize their careers than give additional funding to the senior women of previous generations. $203m was allocated from NHMRC’s prestigious Investigator Grant scheme in 2022 to provide 79 senior grants with a success rate of 21.8 percent, compared to only $107m for 117 early career grants with a success rate of 14.9 percent. If funding of earlier career researchers was made the greater priority, this would have the indirect effect of boosting funding to female researchers.
I am an older male researcher who has had a very good run of NHMRC funding. I also work with many talented younger researchers (mainly women) who are desperate to get funded. From 2019, I decided to make way for younger generations and no longer apply for NHMRC salary funding. Since that time, I have continued to work full-time in research in an Emeritus position using superannuation as my sole source of income. When NHMRC introduced its Investigator Grant scheme in 2019, there was an option to apply for research funding without a fellowship salary, which I successfully did at the most senior level of the scheme. All the Investigator Grant funds I was awarded have been used to support the salaries of younger researchers, who all happen to be female.
The NHMRC gender equity policy has focused on one aspect of gender equity, in an attempt to adjust success rates to give equal number of grants and amounts awarded to female and male applicants. However, in other areas, NHMRC has remained curiously gender blind. The organization regularly publishes data on the amount of funding allocated to various research topics, including women’s health and men’s health. Over many years, funding for research on women’s health has exceeded funding for men’s health by a factor of five-to-one. I have no problem with this, but for advocates of gender equity it is a curious blind spot.