Euthanasia
The Case Against ‘Medical Assistance in Dying’
Canada’s assisted-death law seems connected to the atomization of our society—as much a symptom of inhumanity as a cause.

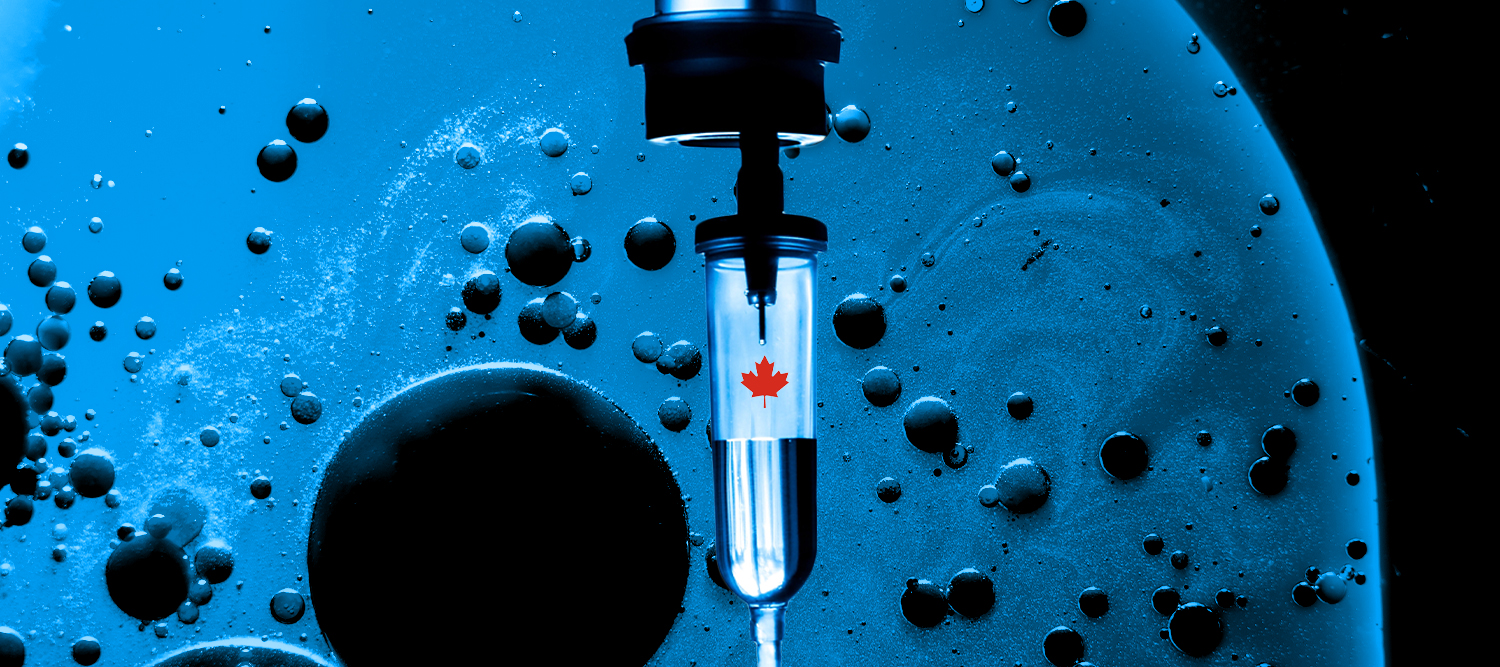
Canadian law now permits something called “medical assistance in dying.” This practice, to be clear, is not palliative care. It does not refer to helping Canadians as they journey toward natural death by offering treatment to manage their pain and suffering. Medical assistance in dying—assisted death for short—is the deliberate act of ending a person’s life, typically through the administration of a lethal substance.
Assisted death is a term that encompasses two distinct categories: euthanasia, where an authorized healthcare practitioner administers a lethal substance, and medically-assisted suicide, where the patient self-administers a substance provided by the practitioner. Both are now legal in Canada if a person meets the statutory criteria to qualify for assisted death, the nature of which will be explained in this article.
The subject presents something of a moving target: In the less than seven years since assisted death became legal across Canada, its scope has dramatically expanded in a manner that many Canadians find deeply troubling. In a newspaper op-ed published last May, I called assisted death in Canada a “runaway train.” For the most part, I still subscribe to that view, though I also believe there is an emerging consensus across ideological lines that we need to get this train back on track. And the federal government appears to be listening. In recent weeks, it legislated a one year delay in the enactment of provisions that would allow assisted death “in circumstances where the sole underlying medical condition identified in support of the request for medical assistance in dying is a mental illness.”
But before discussing how reform might be implemented, it’s worth exploring how Canada originally became a haven for assisted death. That part of the story starts in 2015, when the Supreme Court of Canada unanimously concluded that the country’s absolute criminal prohibition of assisted suicide violated the Canadian Charter of Rights and Freedoms, which forms parts of our constitution. In a case known as Carter v Canada (AG), the Court struck down applicable portions of the country’s Criminal Code to such extent as those portions served to “prohibit physician-assisted death for a competent adult person who (1) clearly consents to the termination of life and (2) has a grievous and irremediable medical condition (including an illness, disease or disability) that causes enduring suffering that is intolerable to the individual in the circumstances of his or her condition.”
You could tell where the Court was headed after reading the ruling’s first paragraph:
It is a crime in Canada to assist another person in ending her own life. As a result, people who are grievously and irremediably ill cannot seek a physician’s assistance in dying and may be condemned to a life of severe and intolerable suffering. A person facing this prospect has two options: she can take her own life prematurely, often by violent or dangerous means, or she can suffer until she dies from natural causes. The choice is cruel.
Under the provisions set down by the Court, Parliament was ultimately granted a year-and-a-half to remedy the identified breach of rights. Legislators responded in June 2016 with what I believe many Canadians—including perhaps some of those who cheered the Carter ruling—expected (falsely) would be the definitive version of Canada’s assisted death law.
Whatever one may think of assisted death, it should be said that Canada’s 2016 law was viewed by many as being consistent with the Court’s 2015 language with respect to what the Charter of Rights and Freedoms requires. The law was also consistent with the desire of many Canadians to have access to what is commonly described as “dying with dignity”—which is to say, assisted death in cases in which a patient is in fact dying, or when death is on the horizon, not when the death of a person is far off or unforeseeable.
This is why the 2016 legislation specifically restricted the decriminalization of physician-assisted death to cases where natural death is “reasonably foreseeable.” Mental illness alone was not deemed a sufficient basis for access to assisted death.
(It is also worth noting that the legislation permits only “medical practitioners” and “nurse practitioners” to provide assisted death. The first category refers essentially to licensed physicians, and the second to registered nurses with specific skills and training. The legislation identifies assisted death as an exemption from what, depending on circumstances, would otherwise be the crime of assisted suicide or culpable homicide. It is therefore a crime for individuals who do not meet the statutory definition of these roles to provide assisted death, even if the person who wishes to die satisfies the criteria to qualify for assisted death.)
Before the ink had dried, however, fresh lawsuits were initiated to challenge the law’s reasonable-foreseeability requirement. In a 2019 ruling, a Quebec Superior Court judge handed two of these litigants a victory, ruling that the country’s 2016 assisted death law must be extended to competent and consenting adults whose suffering is intolerable, and whose illness is incurable, regardless of whether natural death is on the horizon. Rather than attempt to appeal that ruling all the way to the Supreme Court—as many disability organizations urged—the federal government opted to codify the essence of the ruling into what can be called the second version of Canada’s assisted-death law, which was enacted in March 2021. Less than four years after Canada first legalized assisted death, a great bioethical leap in its own right, we expanded the practice to encompass those experiencing intolerable and irreversible suffering at any stage of adult life.
In addition, this second version of the law foreshadowed what might be termed the third (though yet to be realized) version, as it specified that two years later, assisted death would be accessible by adults suffering only from mental illness. This change was scheduled to take effect in March 2023. In December of last year, however, the government announced that it would delay but not abandon this move. As alluded to above, the government made good on this announcement last month, with legislation stipulating that assisted death for adults suffering solely from mental illness will not come online until March 17th, 2024.

But it’s not clear that even this will be the final frontier. A few months ago, a representative from the Quebec College of Physicians told a parliamentary committee studying the future of assisted death that the practice should be expanded to include infants with severe illnesses. Such a step would not only render what is currently considered infanticide legal in some cases, it would also mark an official abandonment of consent as a guardrail in the provision of assisted death, given that newborns and infants cannot meaningfully consent to death.
Moreover, the same parliamentary committee recently recommended that “mature minors” should be eligible for assisted death, and that certain Canadians should be able to provide consent to assisted death before they actually experience the medical circumstances and suffering that would render them eligible to die in this way. And so Canada is at a critical juncture: As the practice is further and further expanded on various fronts, it will naturally become more difficult to explain why the practice shouldn’t simply be granted to anyone who wants to end his or her life, no matter their reason or circumstances.
Writing for Quillette in February, Margaret Wente recently offered a set of sobering “cautionary tales” that illustrate how the boundaries of assisted dying are being expanded to individuals whose primary hardships in life are not so much medical as socioeconomic. These examples serve to vindicate those who’d warned Canada’s Supreme Court Justices that opening the door to assisted death might easily take us down a moral “slippery slope.” In their Carter decision, the Justices addressed such concerns by noting that Canada has a “very different medico-legal culture” than European countries that had already embraced troublingly expansive assisted death regimes. The Justices, like many other Canadians, failed to grasp that culture isn’t static: Through the act of legalizing assisted death itself, we radically reshaped our culture in a way that made the unthinkable suddenly seem thinkable.

Many assisted-dying proponents would freely concede the abrupt nature of this Canadian culture shift, but also describe it as a welcome development—on the view that a swift and radical policy swing was exactly what Canada needed to liberate its citizens from (in their view) retrograde views on death and dying. I very much take the opposite view. I believe that assisted death, in any form, is the wrong choice for a society, with Canada’s experience serving as a case study. The legalization of assisted death as healthcare implicitly teaches us that human life is a depreciating asset with a “best before” date. Even in its most strictly confined form, it contradicts the principle that sits at the heart of a civilized society: human dignity—each person’s intrinsic worth and value—never disappears, no matter how dire our circumstances.
Legalizing—and normalizing—assisted death creates the risk that persons who do not truly desire to die in this manner will nonetheless decide to do so. In fact, government statistics suggest that this may already be happening. Among Canadians who died via assisted death in 2021, nearly 36 percent cited “perceived burden on family, friends or caregivers” as forming part of their decision, and around 17 percent cited “isolation or loneliness.” While these Canadians also would have had to point to some irremediable medical condition causing them profound suffering in order to qualify for assisted death, it appears we’re witnessing situations in which non-medical factors, including the actions, feelings, and emotions of third parties, are motivating people to receive assisted death.
We have seen stories of Canadians facing homelessness, or who cannot find adequate housing, opting to pursue assisted death because they believe they have reached a dead end in life. We have seen stories of military veterans seeking assistance for post-traumatic stress disorder, only to have a bureaucrat suggest assisted death as an option to consider. We are now far beyond what the Supreme Court contemplated in 2015 when its Justices described assisted death as a “carefully-designed system imposing stringent limits that are scrupulously monitored and enforced.”

In 2022, the media reported on two women who’d requested assisted death due to obstacles preventing them from obtaining housing that would protect them from their claimed chemical sensitivities. One of the women, 31 years old and living in Toronto, had already been able to obtain one of the two required approvals from healthcare professionals that the law requires. (Later, she received the second approval.) The other woman, aged 51 years old, had already died via assisted death. Both women suffered from Multiple Chemical Sensitivity (MCS), a controverted diagnosis that many doctors believe is psychosomatic. As one set of published researchers delicately put it, “no clear link has emerged among self-reported MCS symptoms and widely accepted objective measures of physiological dysfunction.”
To put matters into perspective, California legalized assisted death in 2016—the same year that Canada’s first assisted-death regime originally came online. The populations of California and Canada are roughly comparable. In 2021, 486 people in California died via assisted death. In Canada, the corresponding figure was more than 10,000. Nearly all of these deaths were instances of euthanasia: “fewer than seven” were instances of medically-assisted suicide.
One reason for this disparity is that California’s law has always required that those dying by assisted death are terminally ill—a requirement that Canada had originally implemented, but then eliminated within a few years. However, even during the period when the two systems were supposed to be operating on similarly restrictive eligibility criteria, Canada had much higher numbers. In 2016, more than 1,000 Canadians died via assisted death—more than double the number in California that year. By 2020, the last year in which the original terminal-illness requirement was still in place, there were around 7,600 assisted deaths annually in Canada, more than an order of magnitude above California’s tally (495).
In a detailed article published last December in New Atlantis, Washington-based freelance writer Alexander Raikin described the factors that seem to have contributed to these high Canadian numbers: doctor-shopping for assisted death approvals, subjective and flexible interpretation of the law’s eligibility requirements, and inadequate monitoring by government authorities. He also notes that the federal government has largely outsourced the implementation of assisted dying to many of the same medical professionals who agitated for the legislation in the first place, so that “the people doing the training, the assessments, the procedure, and informing the review are all the same people.” Prominent Vancouver-based assisted-death advocate and provider Ellen Wiebe, for instance, reports that helping people end their lives is “the most rewarding work we’ve ever done.”
Canada’s Minister of Justice, David Lametti, claims the Supreme Court has concluded that it would be unconstitutional to exclude persons suffering solely from mental illnesses from accessing assisted death. But this is at the very least a questionable—indeed, I would say incorrect—characterization of the facts. In 2015, the Court expressly noted that its ruling did not encompass assisted death for “persons with psychiatric disorders.” And no lower court in Canada has specifically concluded that legalizing assisted death for persons suffering solely from mental illness is required under the Charter of Rights and Freedoms. For that matter, as discussed earlier, it’s far from clear that the Supreme Court concluded that assisted death is mandated under any circumstances in which a patient isn’t already approaching the end of his or her natural life.
Last Fall, Quebec fashion retailer Simons released a three-minute video showcasing Jennyfer Hatch, a 37-year-old woman from British Columbia who wished to end her life through assisted death. Hatch had been suffering from Ehlers-Danlos syndrome, a condition that affects the connective tissue in the body. The video, which disappeared from the Internet several weeks later following a massive backlash, was entitled All is Beauty. It features images of people on beaches, at one point making mention of “the most beautiful exit.”

It turned out that Hatch, who’d died via assisted death the day before the video was released, had told friends and family that she wanted to live—but for years could not manage to locate appropriate care for her condition. Meanwhile, a Simons executive tried to present the video as a service to Canadian society. “I think we sincerely believe that companies have a responsibility to participate in communities and to help build the communities that we want to live in tomorrow, and leave to our children,” he told the media.
Last December, Ross Douthat of the New York Times wrote a stinging critique of assisted death in Canada, using the Simons video and its gauzy aesthetics as a point of entry. For Douthat, the video teaches that we should “believe in the holiness of euthanasia.” He suggests that Canada is losing its status as a civilized society, arguing that it is “barbaric” to “establish a bureaucratic system that offers death as a reliable treatment for suffering and enlists the healing profession” in such a project. “When 10,000 people are availing themselves of your euthanasia system every year,” he concludes, “you have already entered the dystopia.”
My Sunday column: What Euthanasia Has Done to Canada:https://t.co/ydurBS7o2O
— Ross Douthat (@DouthatNYT) December 4, 2022
So is Douthat correct? Have we Canadians already entered a “dystopia”? I believe the answer is no. Yes, Canada is going down a profoundly troubling path. But there is still time to turn things around by rejecting the normalization (and even celebration) of assisted death, and replacing it with a fervent commitment to providing proper support, care, attention, and resources to fellow Canadians. Imagine if all the time and resources spent on assisted death were directed toward the support, treatment, and care that many of the people pursuing assisted death say they cannot access. This is a choice available to us, just as choosing to go down the road of a highly permissive regime of assisted death was a choice.
Some will say that our constitution, and the Supreme Court’s interpretation of it in Carter, has forced our hand. As a constitutional scholar, I certainly can’t ignore the reality of the Supreme Court’s pronouncements on the subject of assisted death. But because there’s been no pushback from the federal government (even when it came to a lower-court judgment in Quebec that might have been appealed) there is a lack of clarity on what is actually required. For my part, I am skeptical that the Charter’s right to “life, liberty, and security of the person” guarantees the broad right to assisted death that now exists under current law.
Moreover, constitutional exegesis does not take place in a vacuum. What we have witnessed since opening the door to assisted death provides a strong basis for arguing that the associated risks—even in regard to the original law implemented in 2016—are simply too great to justify a breach of the absolute prohibition on assisted death that once existed in this country. The Supreme Court has said that it is appropriate to revisit past decisions where there has been a change in circumstances or evidence that fundamentally shifts the parameters of the debate. Perhaps the story of assisted death now falls into that category.
One path forward would be for the federal government to ask the Supreme Court to issue an advisory opinion in regard to what forms of assisted death are mandated by the constitution. To the extent that the constitution does not demand certain forms of assisted death, politicians and lawmakers would have to make their case for these on grounds other than the alleged need to be constitutionally compliant. I believe the profoundly troubling signs we have already seen in the short history of assisted death in this country would make that case difficult to make.
Beyond the possibility of making a U-turn on assisted death at the level of federal law, there is work to be done at the individual level. It is hard to escape the sense that my country’s drift into a laissez-faire approach on assisted death is connected in some way to the atomization of society. This atomization has been driven not only by the isolation inflicted by COVID, but the more general hyper-individualistic belief that, beyond our close circle of family and friends, we are islands, unconnected to one another. This state of mind lends itself to the idea that if our neighbour is sick, lonely, depressed, and poor, and therefore decides life isn’t worth living, well then, so be it—it’s his decision. What if all of us were to take even a few small steps to reduce the suffering of others?
This may all sound sentimental. But, surprising as this may be to hear from a law professor, law is not the be all and end all when it comes to remedying social illness. First and foremost, it is up to civil society to build up and sustain the ingredients of daily life that facilitate human flourishing and the common good. Canada’s assisted death law, therefore, might be seen as being as much a symptom of inhumanity as a cause.
Consider what happened following media reports of Amir Farsoud, a 54-year old man in Ontario with severe and chronic back pain, facing the prospect of homelessness. He was living with two others in a house that had been put up for sale, and couldn’t find anywhere else to live that he could afford.

Faced with this prospect, Amir decided he would pursue assisted death if he ended up on the streets. As he put it, “I don’t want to die but I don’t want to be homeless more than I don’t want to die.” At the time his story was first reported, Farsoud had received one of the two doctor approvals he needed for assisted death. But shortly thereafter, a crowdfunding initiative raised more than $60,000 to support Farsoud.
As heartening as it is to witness this outpouring of support for a single person, one cannot help but feel a piercing sadness for the many other Canadians who find themselves in similar circumstances, and who either will, or have already, sought assisted death.
I will conclude by sharing a recent experience that struck me to the core. I recently attended a Vancouver Canucks hockey game, and as is customary before the game the crowd rose to sing the national anthem. During the singing of O Canada, I was particularly moved by the line that appears three times in the English version: “O Canada, we stand on guard for thee.” I have often thought of this line in terms of national defence: standing on guard for Canada in times of war.
But on this occasion, in hearing these words, they hit me in a different way. We have an obligation to stand on guard for each other. And as the rise of assisted death shows, we are—in my opinion—failing in a profound way to discharge this obligation. As more and more of our fellow Canadians are offered assisted death as a solution to hardship, this country correspondingly loses its ability to call itself a humane or, as Ross Douthat put it, a civilized society.
This article is adapted from a lecture given by the author on February 2nd, 2023 at Regent College in Vancouver, during an event organized by the James M. Houston Centre for Humanity and the Common Good.