Health
‘It works! It works! It works!’: Jonas Salk and the Vaccine that Conquered Polio
Americans turned on their radios, department stores set up loudspeakers, and judges suspended trials so that everyone in the courtroom could hear what Francis was about to say.

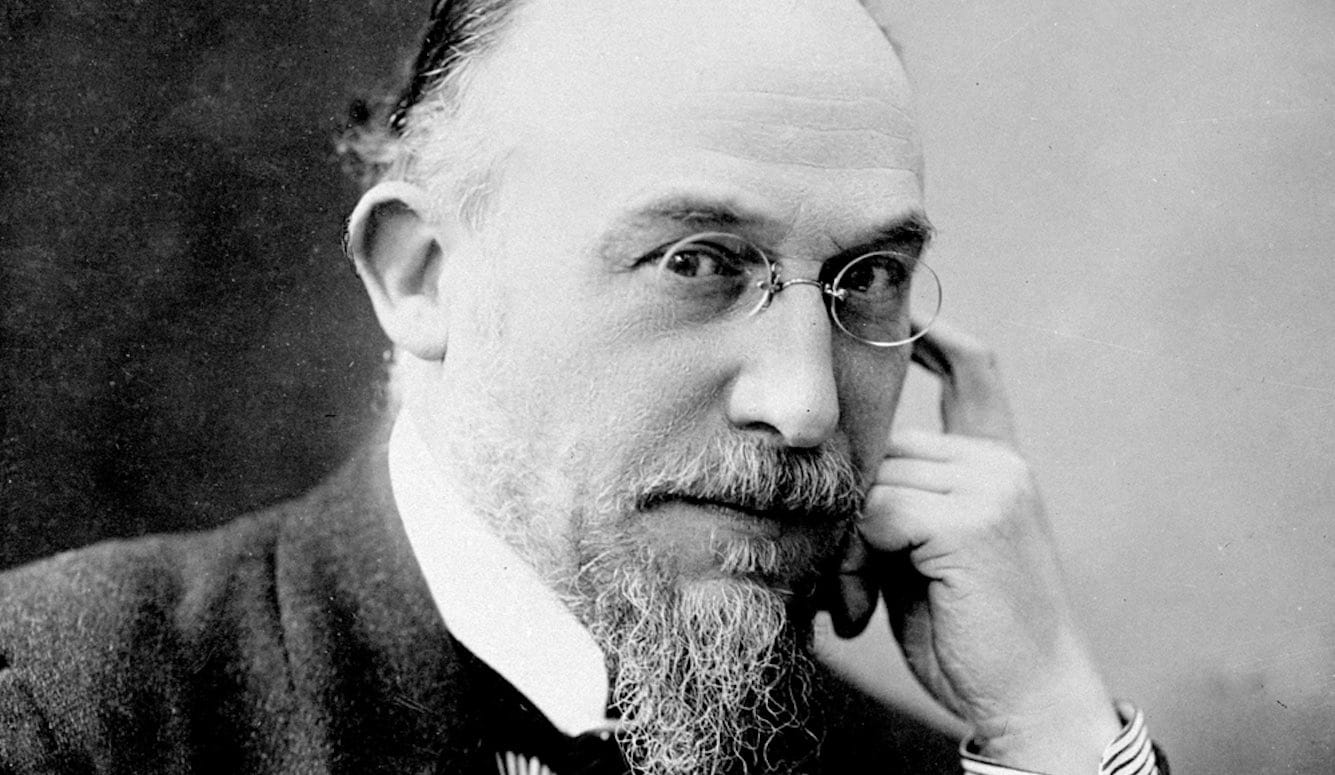
Jonas Salk was born on October 28th, 1914, in a tenement in East Harlem, New York—the first son of Russian immigrants and the eldest of three brothers. After finishing four years of high school in three, Salk entered the City College of New York and later won a scholarship to the medical school at New York University. In December 1941, after the United States entered World War II, Salk was given a choice. He could either be commissioned as a doctor in the armed forces or remain in the United States to pursue a scientific career. He chose science, working on an influenza vaccine in the laboratory of Dr. Thomas Francis at the University of Michigan. Fifteen years later, Francis would supervise the critical test of Salk’s vaccine.
In 1943, while Salk was working on the influenza vaccine, 10,000 people, mostly children, contracted polio in the United States; in 1948, when Salk was first studying polioviruses at the University of Pittsburgh, 27,000 more people were affected; and in 1952, when Salk was first testing his polio vaccine in and around Pittsburgh, 59,000 more cases occurred. A national poll found that polio was second only to the atomic bomb as the thing Americans feared most. There was a desperate, growing desire to prevent polio.
Viruses, unlike bacteria, grow inside cells. To grow polioviruses in the 1930s, scientists John Kolmer and Maurice Brodie had used cells from monkey brains and monkey spinal cords. Salk, on the other hand, used cells from monkey testicles. Later, concerned that people would never accept a vaccine grown in monkey testicles, Salk switched to monkey kidney cells, which are still used to make polio vaccines today.
Because three different types of poliovirus cause disease, Salk knew that he would need to include representatives of all three types in his vaccine. For type 1, Salk chose the Mahoney strain—a decision that would haunt him for the rest of his life. The Mahoney strain was first recovered from a child in Akron, Ohio, whose last name was Mahoney. But the Mahoney strain wasn’t limited to the Mahoneys. The Klines, living next door, were also infected. Three of five Kline children were paralyzed and later died from the disease—an early clue to the unique horror of this particular strain. The other two strains of virus contained in Salk’s vaccine, representing types 2 and 3, weren’t controversial.
The Mahoney strain had one more characteristic that made it particularly dangerous. Although all strains of poliovirus paralyzed monkeys after injection into their brain or spinal cord, only a few strains paralyzed monkeys after injection into their muscles—the route by which children would soon be inoculated. After intramuscular injection, the Mahoney strain was 10,000 times more likely to travel to the brain and spinal cord than any other polio strain. By choosing Mahoney, Jonas Salk was about to jump without a net.
To make his vaccine, Salk took the three strains of poliovirus and, like Maurice Brodie before him, treated them with formaldehyde. To determine how long it took to kill these three viruses, Salk periodically injected them into the brains of monkeys and waited to see if the monkeys would become paralyzed. He found that the viruses no longer paralyzed monkeys after about 10 days of formaldehyde treatment. Then, as a safety measure, Salk treated the viruses for another two days. The strain of virus that took the longest to kill was Mahoney.
To determine whether his vaccine worked and was safe, Salk went to the D. T. Watson Home for Crippled Children. After injecting children with what he hoped would be a safe and effective vaccine, Salk couldn’t sleep. “He came back again that first night to make sure that everyone was all right,” recalled the nurse superintendent. “Everyone was.” The results were disappointing. Salk found that only one of his three vaccine strains induced high levels of protective antibodies in the blood.

In May 1952, Salk tried again. This time, he injected children at the Polk State School, which housed “mentally retarded” boys and men. Unlike the children at D. T. Watson, however, the Polk residents developed immunity to all three types of poliovirus. Also, the vaccine appeared to be safe. “I’ve got it,” Salk said to his wife.
In the spring of 1953, Salk performed the time-honored ritual of vaccinating himself, his wife (Donna), and his three children (Peter, age nine; Darrell, age six; and Jonathan, age three) with his vaccine. “It is courage based on confidence, not daring,” he said. “Our kids were lined up to get the vaccine,” recalled Donna Salk. “I had complete and utter confidence in Jonas.”
To ensure that his vaccine was safe—and that it couldn’t possibly contain live poliovirus—Salk relied on a mathematical model that would soon become controversial. He called it the straight-line theory of inactivation, and it would be at the center of the tragedy that would soon follow. The straight-line theory defined exactly how long it took to completely kill every single particle of live poliovirus. Salk was certain that he could avoid the tragic mistakes made by Kolmer and Brodie.
Here’s how Salk’s straight-line theory of inactivation worked: One dose of the vaccine given to children at the D. T. Watson and Polk schools was about one-fifth of a teaspoon. Salk showed that the quantity of live poliovirus contained in one dose before treatment with formaldehyde was about one million infectious virus particles. Treatment with formaldehyde caused the quantity of live virus to decrease steadily, predictably, and exponentially. After treatment for 12 hours, the quantity of live virus was 100,000 infectious particles; after treatment for 24 hours, 10,000 infectious particles; and after treatment for 72 hours, only one infectious particle remained— the other 999,999 had been killed by formaldehyde. In other words, the amount of live virus contained in the vaccine had been reduced one-million-fold in three days.
When Salk plotted the quantity of live virus against the length of time that virus was treated with formaldehyde, the points connected in a straight line. Salk reasoned that if the virus was treated for three more days, and the line remained straight, then another million-fold reduction would occur. Now, instead of having one infectious particle in one dose, there would be one infectious particle in one million doses. Treatment for another three days would then reduce the quantity of live virus to one infectious particle in one trillion doses—more vaccine than would be required to vaccinate everyone living on the planet. For all practical purposes, treatment for nine days would completely inactivate poliovirus. All this, of course, assumed that the line remained straight. For several years after the events that would follow in the spring of 1955, Salk was the only scientist in the world who believed that his straight-line virus-inactivation curve remained straight.
In 1954, the National Foundation for Infantile Paralysis (otherwise known as the March of Dimes) footed the bill for what would become the largest test of a medical product in history. About 20,000 physicians and health officers, 40,000 registered nurses, 14,000 school principals, 50,000 teachers, and 200,000 Americans in 44 states volunteered. The vaccine was made by two veteran vaccine makers: Eli Lilly and Parke-Davis. Four hundred and twenty thousand children were injected with Salk’s vaccine, 200,000 were injected with saltwater, and 1.2 million were given nothing and merely observed—a total of 1.8 million participants. The choice to include children inoculated with saltwater and children who weren’t inoculated with anything enabled researchers to determine whether the vaccine actually worked.
On Monday, April 26th, 1954, at 9am, six-year-old Randy Kerr of McLean, Virginia, received the first shot. Because the vaccine and placebo injections were coded, neither Randy, his parents, nor the nurse administering the shot knew what he was getting. Randy smiled for the cameras.

During the next five weeks, a series of three shots of vaccine or saltwater was given to first, second, and third graders across the country. Shots were administered in the left arm. Children who participated in the study received a lollipop, a pin that read “Polio Pioneer,” and a chance to avoid the crippling effects of polio. (A trial of this size today would cost about $6 billion.)
The results were encouraging:
- Sixteen children in the study died from polio—all had received the placebo. (This statistic has always haunted me. Had these children not had the misfortune to have been randomized to the placebo group, they could possibly still be alive and well today.)
- Thirty-six children were permanently paralyzed or placed in iron lungs to help them breathe. Thirty-four of the 36 received placebo (a statistic that is equally haunting).
The vaccine worked. But was it safe? Although several cases of polio had occurred within two months of receiving the vaccine, Thomas Francis, the director of the trial, concluded that Salk’s vaccine wasn’t the cause. And he was right—it wasn’t. None of the children were paralyzed in the arm that was inoculated, clearly different from those who once had been paralyzed by the Kolmer and Brodie vaccines. About 420,000 children had been given Salk’s vaccine and not one had been paralyzed by it. The vaccine, apparently, was safe. Now it could be given with confidence.
On April 12th at 10.20am—10 years to the day after the death of polio’s most famous victim, Franklin Delano Roosevelt—Thomas Francis stepped to the podium at Rackham Hall on the campus of the University of Michigan to announce the results of the ground-breaking March of Dimes study. More than 500 people—including 150 press, radio, and television reporters—filled the room; 16 television and newsreel cameras stood on a long platform at the back; and 54,000 physicians in movie theaters across the country watched the broadcast on closed-circuit television. Americans turned on their radios, department stores set up loudspeakers, and judges suspended trials so that everyone in the courtroom could hear what Francis was about to say. Europeans tuned in to Voice of America.
Before Francis presented the results, copies of the report were distributed to the press. “They brought the report in on dollies, and newsmen were jumping over each other and screaming, ‘It works! It works! It works!’” one reporter remembered. “The whole place was bedlam. One of the doctors [had] tears in his eyes.”
When Francis finished explaining that Jonas Salk’s polio vaccine worked and was safe, church bells rang across the country, factories observed moments of silence, synagogues and churches held special prayer meetings, and parents and teachers wept. One shopkeeper hung a banner on his window that read, “Thank you, Dr. Salk.” Newspapers across the country bore the same headline, “Safe, Potent, and Effective.” “It was as if a war had ended,” one observer recalled.
But the war hadn’t ended.
Excerpted, with permission, from You Bet Your Life: From Blood Transfusions to Mass Vaccination, The Long and Risky History of Medical Innovation, by Paul A. Offit. Copyright © 2021 by Paul A. Offit. Published by Basic Books, Hachette Book Group.