Trauma and the Psychedelic Renaissance
Negative stereotypes about psychedelics are undergoing a reassessment.
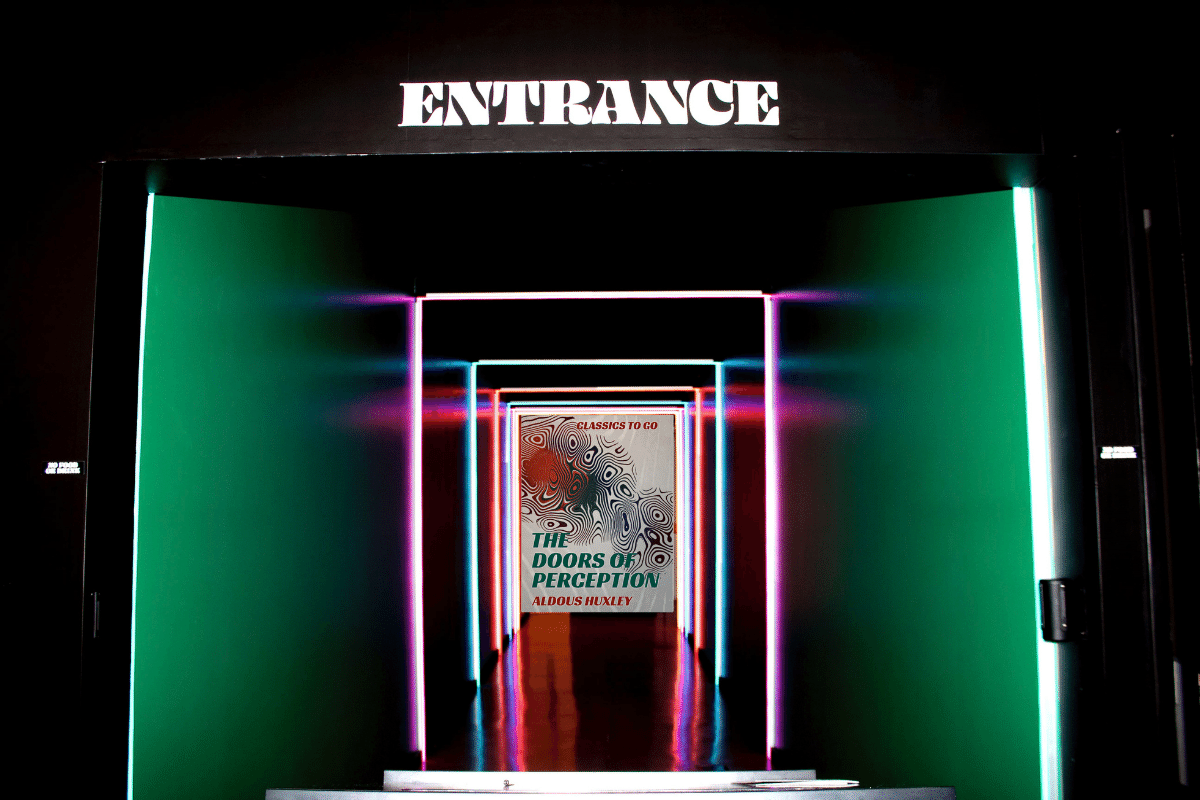
Military veterans with post-traumatic stress disorder (PTSD) and the wildly imaginative British writer and philosopher Aldous Huxley are increasingly finding common ground. In 1954, Huxley published The Doors of Perception, a short monograph detailing his psychedelic experiences on mescaline the previous May, and the book became a bible for the “turn on, tune in, drop out” movement of the 1960s counterculture. Now, the arguments Huxley made in defence of psychoactive drug use are being consulted by doctors exploring innovative ways to treat psychological wounds and mental health problems resulting from military service and trauma. Research into the therapeutic potential of drugs such as MDMA (methylenedioxymethamphetamine) and LSD (lysergic acid diethylamide) collapsed when the drugs were made illegal worldwide in the early ’70s. However, the merits of psychedelic science are currently undergoing an international reappraisal and renaissance, gaining media attention and traction among scientists, doctors, and in the wider public sphere.
Psychedelics first appeared on my radar after I left the British Army in 2010 following tours in Kosovo, Iraq, and Afghanistan. As I wrestled with the fallout of these experiences, I found myself enrolled in a graduate journalism school in the land of Timothy Leary, the American psychologist and counterculture writer made famous by his passionate advocacy of psychedelics during the 1960s. Leary—whom Allen Ginsberg once called “a hero of American consciousness”—had argued that LSD showed potential for therapeutic use in psychiatry. At the time, I was in regular email contact with a friend from the army who had left after our Iraq tour, and we shared concerns over the hair-trigger feelings of volatility we were both experiencing. My friend described it as “The Rage.” Neither of us had known anything like it before, but now it could suddenly surge out of the blue like a Hellfire missile, often in the most mundane situations.
“Especially if there was something on the news about Iraq or Afghanistan, or some stupid film with shooting or violence, I would get extremely agitated and argumentative, generally be unable to sleep and go to sleep on my own on the sofa,” my friend told me. I was undergoing similar experiences and self-medicating through a tawdry combination of far too much alcohol and online pornography. Our frank discussions led my friend to recommend equally frank countermeasures. Among his eclectic list of rage suppressers—including good 19th-century literature, learning to cook tasty organic Mediterranean food, regular sex in a stable relationship, prayer, and the New Testament—he suggested micro-dosing with MDMA (also known as ecstasy) once every six months “just to take the edge off.” My first attempt to follow this advice was a failure—I lost $25 to a fellow student for some MDMA that never materialised. I became discouraged but some years later, at the Electric Forest dance music festival near the small town of Rothbury, Michigan, I found a more reliable source, although the psychedelic on offer this time was LSD. “Be careful—you’re about to discover everything they told you is a lie,” my friend advised as I placed the tiny piece of paper under my tongue. The experience proved revelatory.

Negative stereotypes about psychedelics are undergoing a reassessment. A new US study demonstrates that MDMA can bring relief to those suffering from severe PTSD when combined with talk therapy. “Unlike traditional pharmaceuticals, MDMA does not act as a band-aid that tries to blunt symptoms of PTSD,” the New York Times reported. Rather, when combined with therapy, the drug “seems to allow the brain to process painful memories and heal itself.” However, the study found that MDMA does not automatically produce beneficial results when taken without therapy.
Rick Doblin, the study’s senior author and director of the Multidisciplinary Association for Psychedelic Studies, a nonprofit research group that sponsored and financed the clinical trials, told the Times that “It’s not the drug—it’s the therapy enhanced by the drug.” That the study of psychedelics and their application in the treatment of traumatised military veterans is being spearheaded in the US isn’t a surprise. Not only was the country the hub of the 1960s counterculture, but its enormous military has also produced a large veteran population who saw active combat from Vietnam to Afghanistan, and therefore energetic research into PTSD and moral injury. Nor is it much of a surprise that the UK is behind on this, as it is on all veteran-related matters. But the consideration of psychedelic-assisted psychotherapy in Australia is remarkable, given the country’s conservative bent on most things.
The Australian government’s Therapeutic Goods Administration (TGA) is currently evaluating a range of proposals around whether psychiatrists should be allowed to prescribe MDMA and psilocybin—the psychoactive component of magic mushrooms—to treat PTSD and a range of other mood disorders, such as anxiety, depression, and addiction. In July 2020, Mind Medicine Australia filed an application with the TGA requesting that MDMA and psilocybin be reclassified as Schedule 8 controlled medicines. Both substances are currently classified as Schedule 9 prohibited drugs, in the same category as heroin. If they are reclassified, MDMA and psilocybin would sit alongside drugs like dexamphetamine, morphine, and some forms of medicinal cannabis, and Australia would become the first country in the world to consider these drugs as legitimate medicines.
The TGA was due to deliver its verdict on April 22nd, but delayed the decision after it decided “to seek further advice in relation to psilocybin and MDMA” which “will include an independent expert review into the therapeutic value, risks and benefits to public health outcomes for these substances.” Concerns about the medicinal use of these drugs include the current lack of healthcare professionals trained to provide psychedelic-assisted psychotherapy. Doctors need to be able to judge whether the powerful changes in consciousness these drugs can effect could lead to psychological harm, rather than healing, when administered to unsuitable patients. There are also worries that the presently higher costs of pharmaceutical-grade psychedelics would drive things underground, resulting in people accessing unregulated MDMA and psilocybin treatment services, thereby putting them at risk due to a lack of quality control.
Nevertheless, the case for psychedelics is strengthened by mounting evidence that the current drug regime being offered to veterans suffering from PTSD is not working and may be causing serious harm. A recent report by ABC News focused on an Australian veteran, David Hill, who became addicted to the tranquilliser benzodiazepine, prescribed to treat his PTSD after two tours in Afghanistan. At one point, he was taking 50 pills a day. “You may as well just be a walking ghost,” Hill says in the article. “You become numb to just about every emotion, including joy.” As he became dependent on the medication, the drugs ended up making his struggle with PTSD harder. “You just can’t focus on the problem. You can’t identify what the problems are. So it’s just masking the seriousness and all the symptoms that come along with it.”
The article notes that experts say benzodiazepines can be helpful in short periods for treating symptoms of anxiety and insomnia, which is common in PTSD. But in the medium-to-long term, it becomes counterproductive to effective treatment through psychotherapy and other techniques. The gruelling experiences of bestselling Canadian author and academic Jordan Peterson have offered a reminder of the potential perils of benzodiazepine abuse. He recently returned to public life with a new book Beyond Order: 12 More Rule for Life, following rehabilitation from prescription drug dependence which he admits came close to ruining his life.
Hill tried and failed to obtain medicinal cannabis through the Department of Veterans Affairs as a means of helping his PTSD and breaking his benzodiazepine addiction. Eventually his situation became so dire that his father, a former narcotics officer, resorted to illegally obtaining cannabis oil for his son. The drug helped wean Hill off benzodiazepine and “begin a more meaningful period of treatment for PTSD.” Hill concludes that there was not enough education for discharged veterans about what assistance was available, or a willingness to talk about the issues confronting those returning from war.
Hill’s observation—which chimes with my experiences after leaving the British Army—has added resonance given the mental health issues now fomenting across all strata of society due to the COVID-19 pandemic. In a previous article, I discussed the moral injuries that likely await some health workers due to their experiences during the COVID-19 outbreak. But the mental health of many ordinary people will also have taken a hit. Quarantines and curfews can produce their own negative psychological impacts, including PTSD symptoms, depression, and insomnia. For some who have suffered PTSD before, the general stress of living through the pandemic can resurface past trauma.
Australia’s Black Dog Institute, a leading independent mental-health research organisation, has raised concerns about “a significant minority who will be affected by long-term anxiety.” In the UK, a group of leading public health specialists writing in the British Medical Journal warned that “the mental health impact of the pandemic is likely to last much longer than the physical health impact.” Joshua C Morganstein, assistant director at the US-based Centre for the Study of Traumatic Stress, told the BBC: “Historically, the adverse mental health effects of disasters impact more people and last much longer than the health effects. If history is any predictor, we should expect a significant ‘tail’ of mental health needs that continue long after the infectious outbreak resolves.”
At the same time, others are cautioning against our increasing recourse to diagnosing the likes of PTSD and moral injury. There is concern that the bar for trauma severity set by the mental healthcare industry is getting lower and lower, thereby enabling almost anyone to join the trauma-suffering community. It does seem that we are increasingly told by some expert or commentator from some organisation or other that we inevitably have some form of trauma based on our experiences that we need to acknowledge, share, and discuss. I’m acutely conscious of that trend in relation to my own experiences and decade-long navel-gazing endeavour over Iraq and Afghanistan.

Prince Harry, who also served in Afghanistan, has spoken candidly about his struggles with trauma following the death of his mother and his subsequent recourse to counselling over the last decade. Some are now suggesting he may have overdone the therapy. Correctly discerning what is and isn’t trauma, or what sort of trauma goes beyond the usual levels of stress that are an inevitable part of life and therefore warrant more attention, is a challenge. When you then combine that quandary with the question of whether to medicate with powerful mind-altering drugs, it gets even more complicated.
My own limited experiences with psychedelics—MDMA and LSD—appeared to confirm that their use in treating the likes of PTSD is only really effective when combined with talk therapy. My earlier mind-altering trips were fantastic fun but ultimately failed to make a dent in ameliorating my moral injury. I also found that taking psychedelics on their own carries the usual risk of leaving the user increasingly addled and—especially if there is a mental health issue like PTSD or moral injury crouching in the corner—unable to focus on resolving the real problem. I recently underwent counselling for the first time through the Transition, Intervention, and Liaison Service (TILS) provided for British veterans by the UK’s National Health Service (recently renamed Op Courage: The Veterans Mental Health and Wellbeing Service), which I can heartily recommend. During this period, I dropped acid in between counselling sessions—not, I must emphasise, with any prompting from or even any knowledge on the part of my counsellor. While this was not a controlled application of psychedelics with talk therapy, I nevertheless found the experience beneficial in ways that my purely recreational use was not. While I can’t draw any firm conclusions from my own experiences, they suggest that continued scientific inquiry in this area may yet yield further promising results and help alleviate the mental trauma I and others have been struggling to manage.
As for Aldous Huxley, by the end of his life he had fully embraced the ameliorative powers of mind-altering drugs—on his deathbed on November 22nd, 1963, he famously took a final dose of LSD so he could enjoy one last trip. But earlier in his life he had harboured concerns about drugs (an inversion of the usual dynamic of society’s youth embracing drugs under the disapproving gaze of elders). His most famous novel, Brave New World, published in 1932, is set in a dystopian scientific dictatorship in which citizens are rendered docile by the government-supplied drug soma that enables them to “take holidays from their black moods, or from the familiar annoyances of everyday life,” while softening their minds and poisoning their bodies. The book culminates with its protagonist rebelling against the oppressive system, directing his anger in particular at the production of soma, which has come to symbolise all that is rotten in the chemically managed future state. Come Christmas Eve, 1955, though, Huxley took his first dose of LSD. After which he saw things differently.