COVID-19 Updates
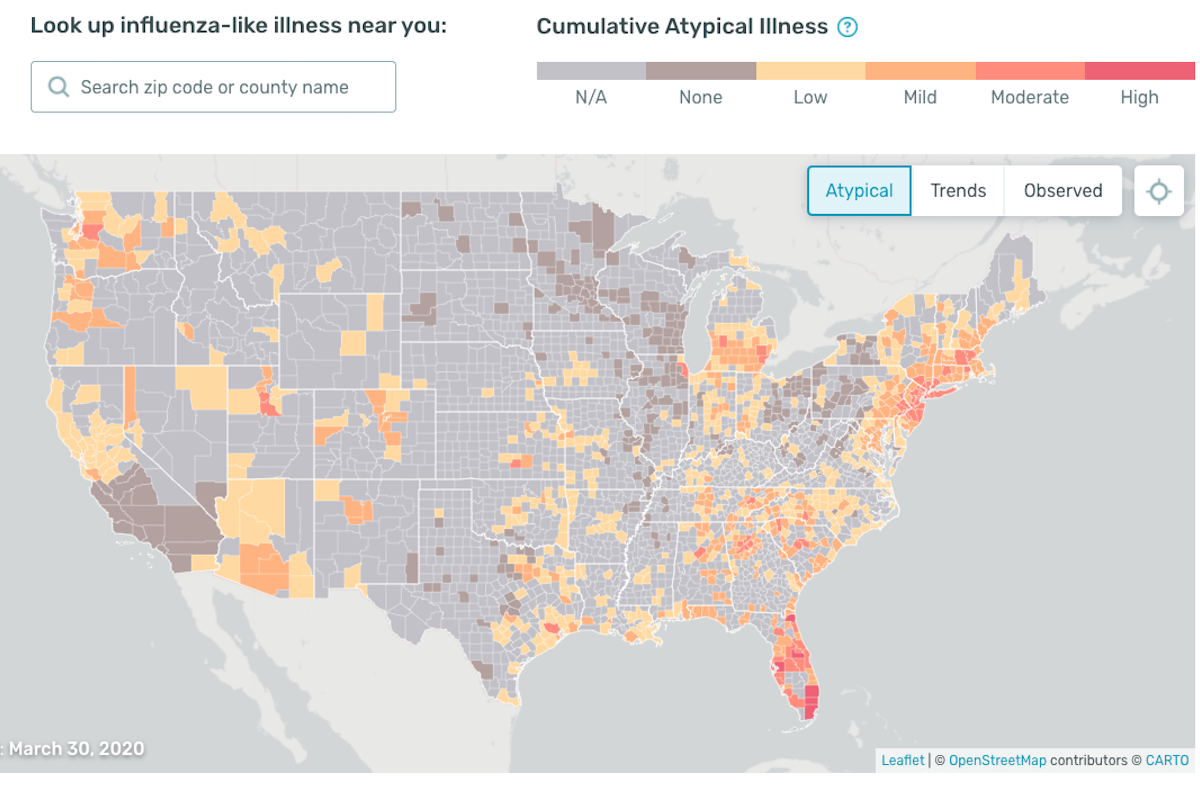
COVID-19 Science Update for March 31st: Wear a Mask, Georgia's SSE, Kinsa's Fever Map
Both the scientific literature and media reports suggest COVID-19 transmission is most likely to take place (1) within families, and (2) through one-off SSEs of the type described above.
This article constitutes the March 31st, 2020 entry in the daily Quillette series COVID-19 UPDATES. Please report needed corrections or suggestions to [email protected].
Today’s data
According to statistics compiled by Our World in Data (OWD), the number of newly confirmed COVID-19 deaths increased yesterday.
The data, as reported by the European Centre for Disease Prevention and Control (ECDC), indicated 3,698 new confirmed COVID-19 fatalities globally, up from Monday’s newly reported deaths, of which there were 3,125. This included 418 new cases in France, 128 in Germany, 28 in Canada, and 661 in the United States—all of which represent new highs for these countries. Italy and Spain recorded 810 and 812 new deaths respectively, roughly equivalent to their average daily values over the last week. As usual, the four countries that consistently registered the most new deaths over the last three weeks—France, Italy, Spain, and the United States—accounted for almost three-quarters of all new deaths worldwide (73 percent).
One other statistical pattern worth noting: Yesterday’s drop in worldwide newly reported deaths—from 3,461 to 3,125—represented the second week in a row during which a decrease was reported on a Monday, followed by an increase on Tuesday. This may well be a coincidence. But given that these are the only two day-to-day global drops in newly reported COVID-19 deaths over the past two weeks, it also may reflect the anecdotally described phenomenon by which regional and national health authorities sometimes don’t formally report weekend deaths until Monday (which means they don’t get included in publicly listed tallies until Tuesday) .