COV
COVID-19 Science Update for March 22nd: Grim Omens in the U.S.
The problem isn’t just the number of ventilators and ICU beds, but also the limited number of staff who can operate such equipment.

The latest global data for COVID-19—updated with reports received on March 22nd, 2020—have been published at Our World in Data. Here are some of the numbers and trends that I believe deserve special attention, as well as a brief report on notable regional developments and media analyses. Since March 21, these updates have been published at Quillette in our section marked COVID-19 UPDATES. Please report needed corrections or suggestions to [email protected].
Yesterday’s global tally of total confirmed cases was 305,275. This represents a daily jump of 34,047, up from the previous daily jump of 28,891. This includes:
- Another 6.5K cases in Italy (a slight increase from the previous daily jump);
- A worrying 4.9K case jump in Spain (up from the previous daily jump, which was 2.8K);
- And a big 7.1K increase in the United States, the biggest U.S. jump to date.
These three countries account for more than half of all new cases. If you add in France (1.8K) and Germany (3.3K), you get more than two thirds of global cases.
There were 1,690 new deaths reported globally. This includes the following regional developments:
- France had 112 new deaths, and Spain had 324. These countries appeared somewhat in lockstep in early March, with both showing roughly similar increases in daily death tallies. But the last few days have been different: While France has had roughly 100 deaths per day for almost a week (much like Iran), Spain doesn’t seem to be plateauing. The numbers suggest it could become the next Italy.
- Italy itself had 795 new reported deaths, up from 625 the day before, and almost half of the global total. When it comes to the toll this disease has taken, Italy now stands completely apart from other countries—in total deaths (approaching 5,000), known case-fatality rate (an order of magnitude above the level observed in South Korea and, in the latter period, China), and in the sense of chaos and terror inflicted on local residents and health providers (in the Lombardy region, specifically).
- There were 30 new cases in Belgium. That country’s previous total had been just 38, suggesting a pattern similar to Germany, where mortality has remained very low, but has gone up markedly this week (including 22 newly reported deaths in today’s new German numbers).
- Switzerland had 13 new deaths, despite very high new-case numbers over the last two weeks, and its pattern might be tracking Germany and Belgium. By comparison, the UK has 233 total deaths (including 56 new ones), compared to Switzerland’s cumulative total of 56, despite both countries’ new-case totals having initially begun to surge around the same time and at the same rate.
- The United States had 80 new deaths, though for reasons discussed immediately below, that number seems likely to surge in coming weeks.
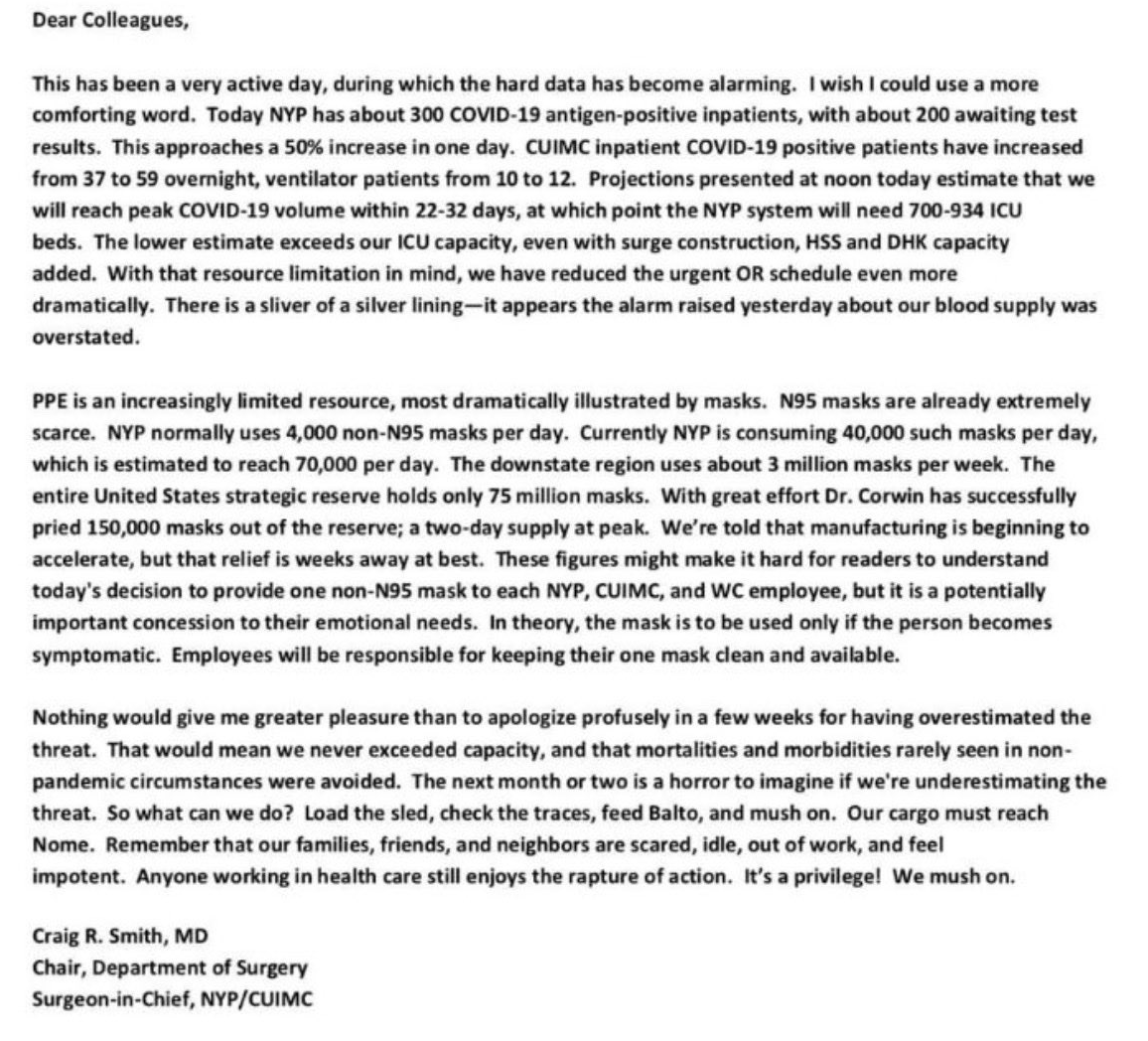
There are many indicators suggesting that the situation in the United States may get much worse before it gets better. Though media attention has focused on the surreal dysfunctionality that characterizes the U.S. political climate, it’s also clear that there’s been poor long-term planning at all levels, especially in the New York City area, where half of all confirmed U.S. cases have been reported. Attached, by way of example, is a screenshot of a social-media post from Craig R. Smith, Chair of the surgery department at New York-Presbyterian/Columbia University Medical Center. You would expect such facilities to be among the best equipped in the world. Yet Dr. Smith notes that his hospital will likely need 70K masks per day, which is about 0.1 percent of the entire national strategic reserve.
In the short-term, these shortfalls will have a tragic human cost. In the long-term, they may even have a geopolitical cost, as U.S. stature suffers amidst the outbreak. As Steven Erlanger notes, many nations are now looking to China for medical assistance, despite Beijing’s early missteps and cynicism when presented with signs of a pandemic brewing in Wuhan.
Until a month ago, if you would have asked me where I would like to get acute medical care for some hypothetical illness, I might have picked New York City, because of its high concentration of elite teaching hospitals and world-renowned medical experts. But as I’ve noted before, this disease has disproportionately afflicted some of the wealthiest nations on Earth—including, in cases such as Lombardy, Seattle, and New York City, some of the wealthiest areas within those wealthy nations.
To take another example: In Switzerland—which many of us might regard as the very epitome of an efficient, rationally organized, well-resourced society—a government official has warned that, as Reuters reports, the “health care system could collapse by the end of the month if the new coronavirus keeps spreading at current rates.” The problem isn’t just the number of ventilators and ICU beds, but also the limited number of staff who can operate such equipment. (I recall that when my own daughter had breathing problems in a hospital setting, a special team was summoned in case she required emergency interventions—doctors and nurses whose technical training was even more specialized than the specialists in attendance.)
On the issue of testing, here’s an interesting case study from Iceland, reported by Buzzfeed. As with other countries that have been successful in quickly rolling out large-scale COVID-19 testing, the government has enlisted at least one private partner (in this case, a firm called deCode Genetics). This has permitted officials to test even those who have no symptoms, thereby giving us a better look at the true baseline infection rate (and, therefore, mortality rate). Of the asymptomatic group—basically a random, voluntary sample of the population—about 1 percent were infected. (Buzzfeed also reports that similar testing procedures have been implemented on a smaller scale in other countries, including in the Veneto region of Italy, but that national-scale testing of non-symptomatic individuals is, for now, simply impractical in any but the smallest countries.)
One apparent bright spot in last month’s Report of the WHO-China Joint Mission on COVID-19 was that the disease was reported as being difficult to transmit in a hospital or other institutional group setting. But new data suggest that enormous numbers of health-care workers in Spain—3,500 by one estimate—have been infected. Also, today’s New York Times has a definitive piece on the Life Care Center nursing home in Kirkland, Washington (a suburb of Seattle):
Since the first positive tests at Life Care came back on Feb. 28, 129 people there—including 81 residents, about two-thirds of its population—have tested positive for the virus, and 35 people have died. Dozens of its workers have received coronavirus diagnoses, suggesting that the center’s frantic efforts to sanitize the building, quarantine residents and shield staff members with gowns and visors may have come too late.
To put one of those numbers in context—35 deaths—that’s about three times the number of deaths that have been reported in all of Canada.
Another Times article presents lessons from Italy, where swathes of Lombardy became one giant Life Care Center: Lots of people raising the alarm, but no central co-ordinated action till too late. The article also highlights the role of what some call “super-spreaders,” including this person:
When a 38-year-old man went to the emergency room at a hospital in Codogno, a small town in the Lodi province of Lombardy, with severe flu symptoms on Feb. 18, the case did not set off alarms. The patient declined to be hospitalized and went home. He got sicker and returned to the hospital a few hours later and was admitted to a general medicine ward. On Feb. 20, he went into intensive care, where he tested positive for the virus. The man, who became known as Patient One, had had a busy month. He attended at least three dinners, played soccer and ran with a team, all apparently while contagious and without heavy symptoms.
Finally, a lot of us have wondered if the weather will bail us out, just as warmer weather in spring signals an end to the winter flu season. The answer, as Nicholas Kristof reports is, we simply don’t know:
Some respiratory viruses decline in summer from a combination of higher temperatures and people not being huddled together, so it is possible that Northern Hemisphere nations will enjoy a summer break before a second wave in the fall. That’s what happened during the 1918 Spanish flu pandemic: It hit in the spring of 1918, went away but returned worse than ever in the fall. Of the four coronaviruses that cause the common cold, two diminish in warm weather, while two are more variable. SARS and MERS did not have clear seasonal variations, and even seasonal flu is transmitted in the summer, although less than in winter. So while experts hope that hot weather will shortly bring a reprieve from the coronavirus—the flu is already on the retreat — there’s no solid evidence.