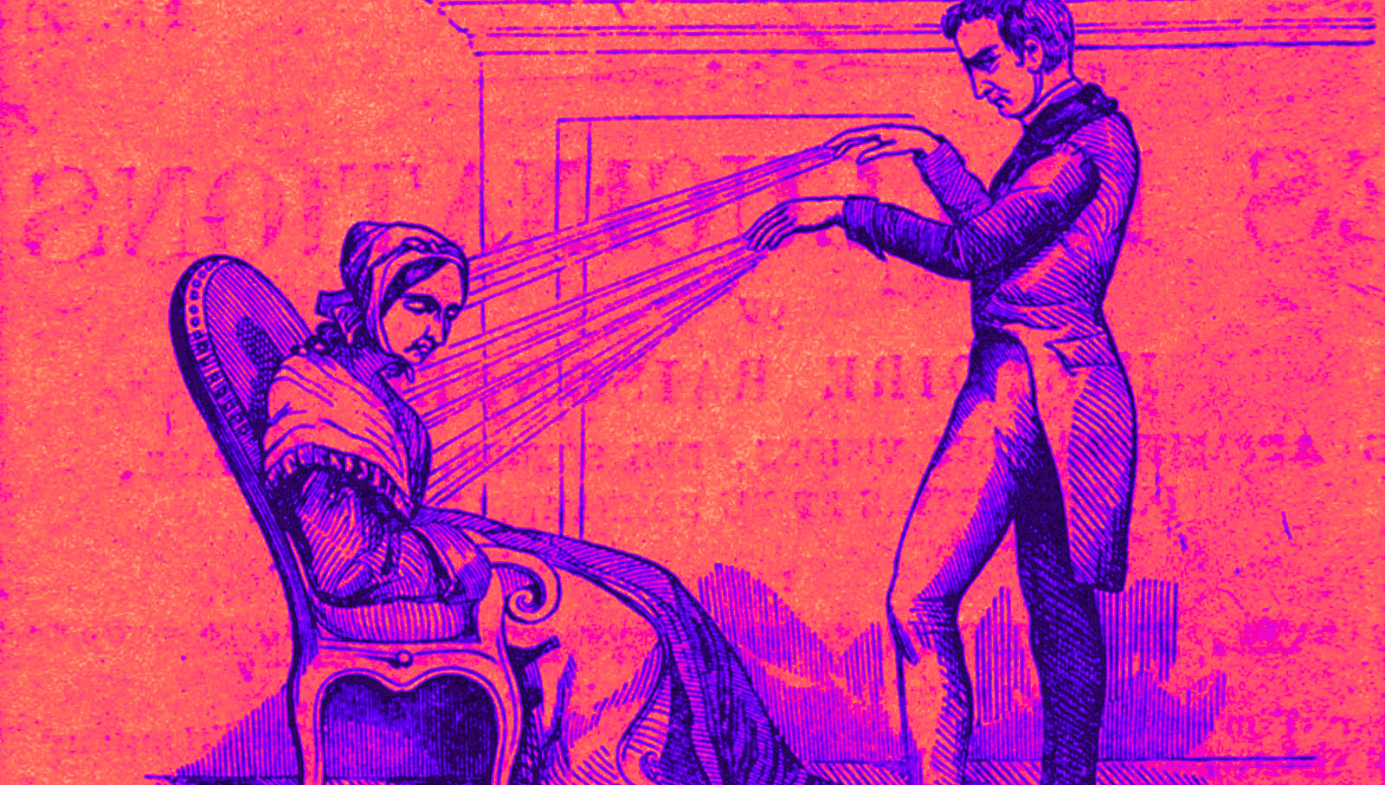
Medicine
The Placebo Effect’s Evil Twin
The Nocebo Effect occurs when we experience pain, depression, or illness based on nothing more than negative expectations.
· 8 min read
Keep reading
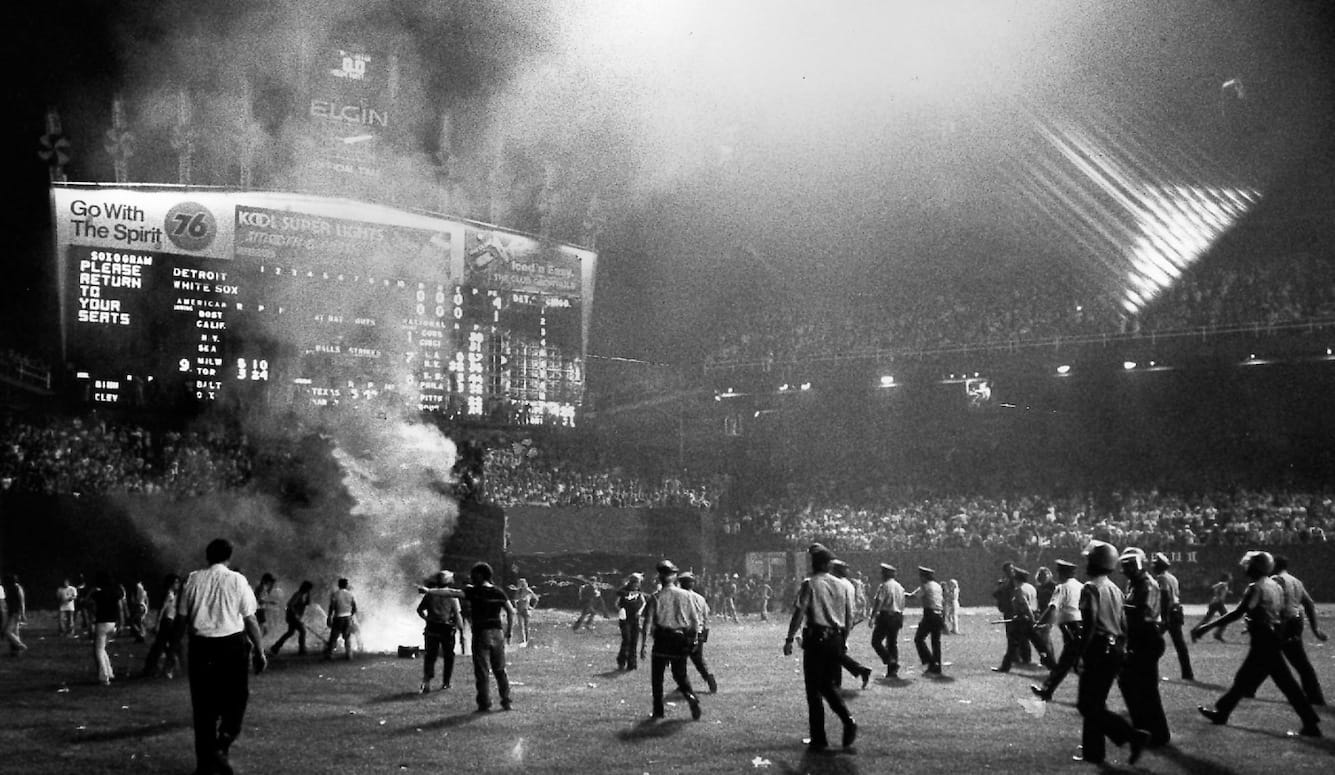
Disco Inferno
George Case
· 10 min read
Conflicting Visions of Peace
Benny Morris
· 8 min read
When Women Are Radicalised
Claire Lehmann
· 8 min read
The First Journalists
Iona Italia, Quillette
· 60 min read
Buckley’s Blind Spots
Ronald Radosh
· 25 min read
The Art of Not Quite Listening
Thomas Larson
· 9 min read