Psychology
When Therapy Makes Things Worse
Spending time with friends and family, exercise, and volunteer work are often more helpful than long conversations about one’s anxieties and grievances.
· 9 min read

Keep reading
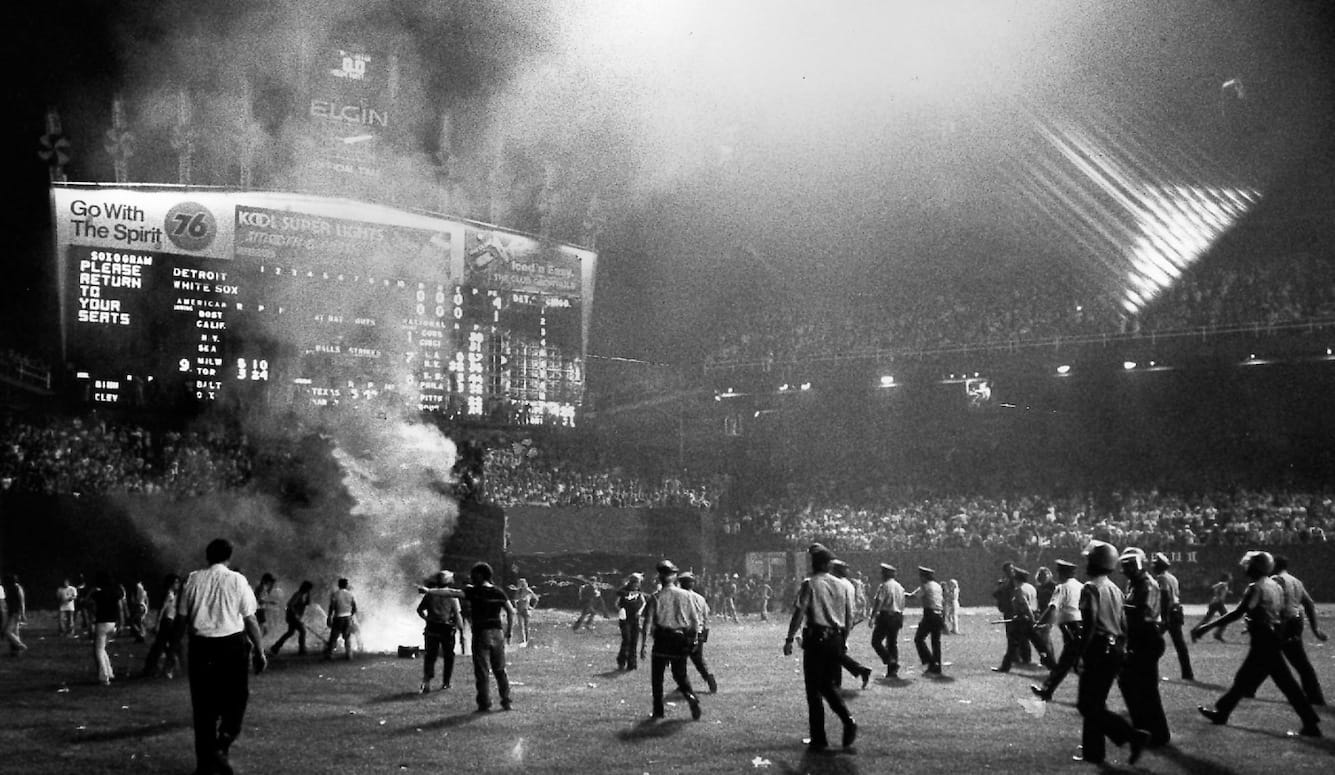
Disco Inferno
George Case
· 10 min read
Conflicting Visions of Peace
Benny Morris
· 8 min read
When Women Are Radicalised
Claire Lehmann
· 8 min read
The First Journalists
Iona Italia, Quillette
· 60 min read
Buckley’s Blind Spots
Ronald Radosh
· 25 min read
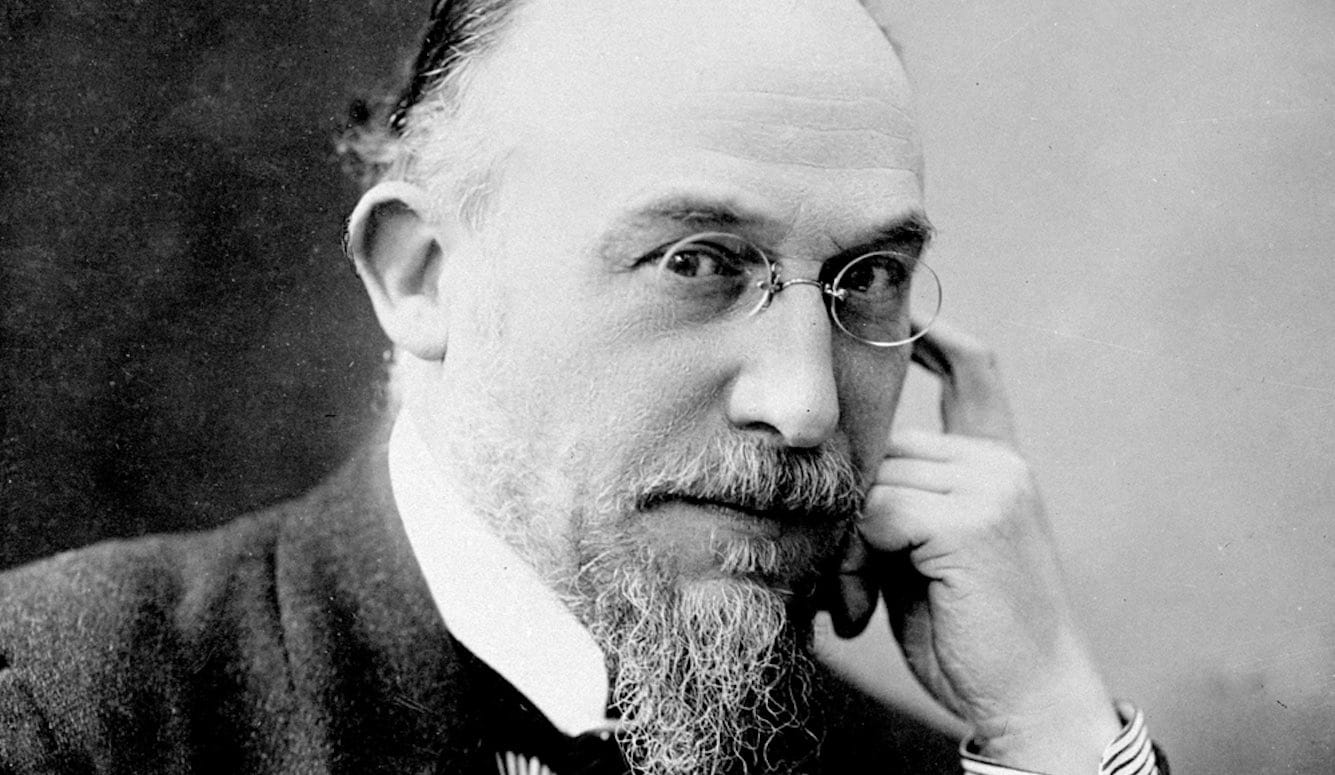
The Art of Not Quite Listening
Thomas Larson
· 9 min read