Science / Tech
Intelligence and Health Outcomes
The importance of cognitive ability to disparities in human health is being overlooked.
· 9 min read

Keep reading
Glamourising Violence at Glastonbury
John Aziz
· 8 min read
From Welfare to Warfare
John Lloyd
· 7 min read
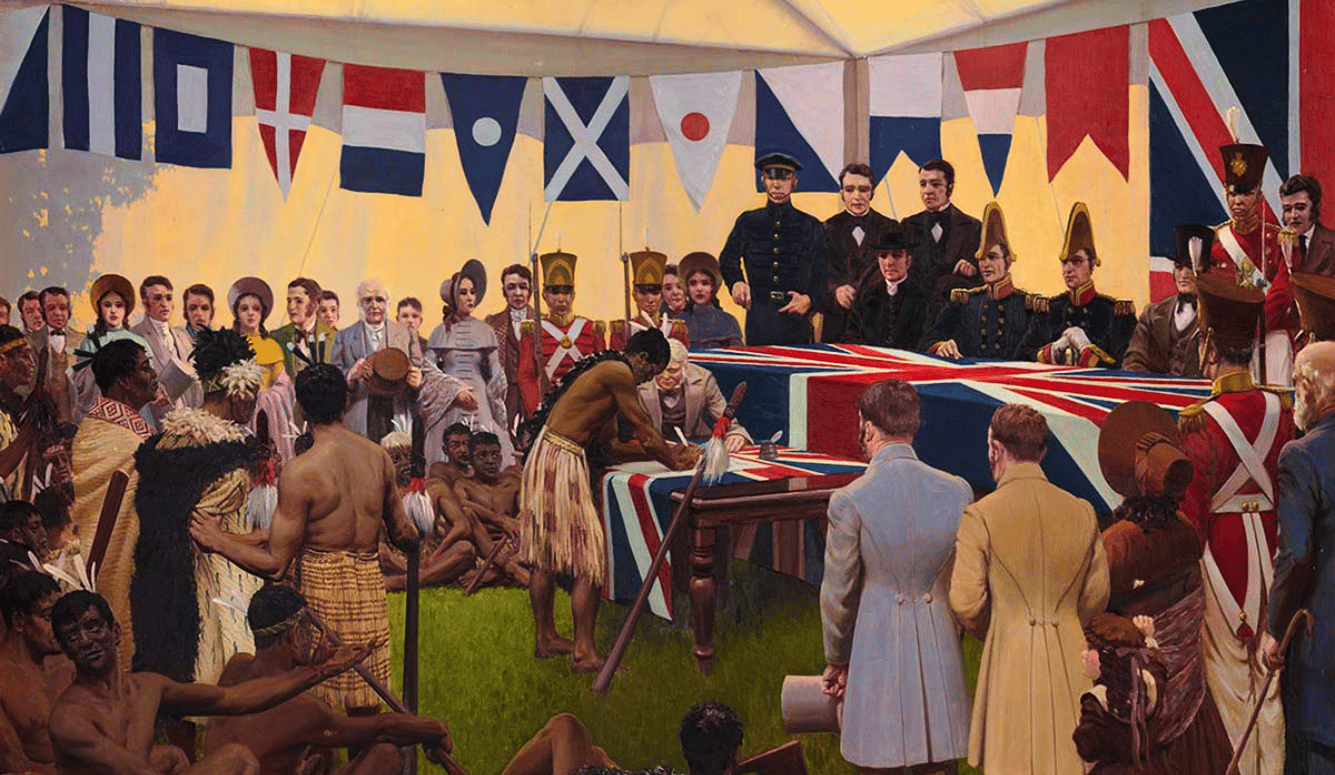
Stealing Australia and Buying New Zealand
Sean Welsh
· 16 min read
After Liberal Internationalism
Matt Johnson
· 21 min read