public health
Masking Uncertainty in Public Health
Had it actually been “following the science,” the CDC would have transparently communicated its uncertainty at every step.
Let’s travel back to simpler times, 2019 and earlier. In the years Before COVID (BC), beliefs about respiratory viruses were not intertwined with people’s core identities. Preventions and treatments could be studied scientifically without people lining up ahead of time to either believe or disbelieve the evidence according to whether it aligned with their political allegiances. Grant-giving agencies were willing to finance high-quality research because they wanted to know the truth about whether or not, or the extent to which, a given intervention could promote health and ultimately save lives.
One such intervention was masks against widely circulating viruses, most importantly influenza. During the final decade BC, the flu on average killed 35,000 Americans annually. Intuitively, one might expect that wearing some kind of face covering would curtail the transmission of respiratory infections. Research in materials science, which focused on the physical characteristics of various fabrics, suggested a benefit. Some observational studies reached similar conclusions.
At the same time, researchers knew that the history of medicine is littered with seemingly plausible interventions whose purported benefits were later disproven. What works in laboratories often fails when tested in natural settings, even when the biological mechanism appears credible. Meanwhile, observational studies are vulnerable to unknown or unmeasured confounding variables. If the people who follow medical advice on a subject engage in other health-promoting behaviors that are impossible to fully enumerate and incorporate into a study, the advice can seem efficacious even when it’s not.
These problems can be solved through Randomized Controlled Trials (RCTs), long considered the gold standard for assessing medical interventions. The field of evidence-based medicine, in fact, emerged because of growing awareness that RCTs yield more accurate results on health interventions than laboratory and observational studies. By randomizing subjects between treatment and control groups, preexisting differences between people are averaged out, allowing scientists to isolate the causal effect (if any) of the intervention. RCTs are widely employed in medicine well beyond pharmaceuticals, including in areas such as acupuncture and surgery that require creativity in constructing the placebo. The case for or against a given intervention is strongest when multiple well-designed RCTs converge on the same conclusions.
Between 1946 and 2019, 10 RCTs tested the effectiveness of community masking for slowing the spread of respiratory infections. Naturally, public health authorities in early 2020 wanted to apply what had been learned to the new threat of COVID. The Centers for Disease Control and Prevention (CDC) therefore highlighted in one of its in-house journals a systematic review of the evidence. Originally published on February 6th, 2020 and republished later that spring, the review reaffirmed what had long been the mainstream position in public health: community masking doesn’t work. In the words of the CDC’s report, “We did not find evidence that surgical-type face masks are effective in reducing laboratory-confirmed influenza, either when worn by infected persons (source control) or by persons in the general community to reduce their susceptibility.”
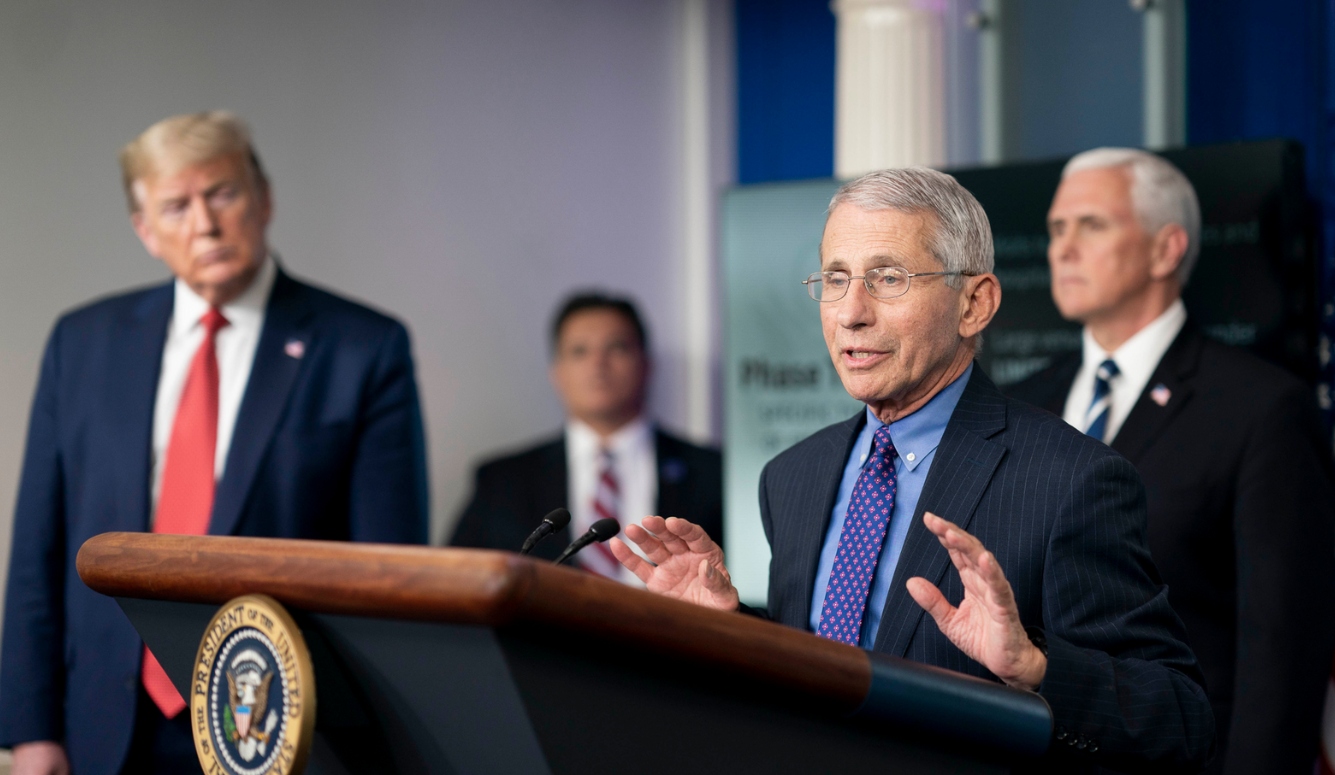
That body of research informed the messaging and policy guidance that public health authorities initially offered on COVID. Although there were dissenters in the academic community, the people holding high-ranking government positions uniformly said that community masking was ineffective and therefore inappropriate as a policy tool. In his appearance on 60 Minutes on March 8th, 2020, Anthony Fauci bluntly told Americans, “There’s no reason to be walking around with a mask.” Fauci also noted the shortage of medical (surgical) masks, and he said the limited supply should be preserved for health care workers. In their tweets, interviews, lengthy press briefings, and testimony before Congress, CDC Director Robert Redfield, Secretary of Health and Human Services Alex Azar, and Surgeon General Jerome Adams all made the same points.
Many Americans nevertheless began buying, making, and wearing masks. It’s not hard to see why so many people found the initial public health messaging unpersuasive. Despite having numerous chances, Fauci, Redfield, Azar, and Adams never invoked the scientific research on masking to explain to the public how they knew it was ineffective. A widely quoted tweet from Adams, for example, simply stated that masks “are NOT effective in preventing general public from catching #Coronavirus.” To the ordinary person, statements of that sort could easily sound like mere assertion rather than a reasonable conclusion from the existing data.
When authorities followed up by saying the limited supplies of masks must be preserved for health care workers, a discerning person might infer that masks actually are effective. Otherwise, why would medical personnel need them? We can safely assume that people wanted doctors, nurses, and others involved in patient care to be protected from the coronavirus, but they also feared for their own lives. Fauci, Redfield, Azar, and Adams did not tell Americans what the CDC’s report affirmed: surgical masks are worn in health care settings not to prevent transmission of respiratory infections, but rather “to protect accidental contamination of patient wounds, and to protect the wearer against splashes or sprays of bodily fluids.”
Less than a month after his 60 Minutes interview, Fauci and the nation’s other public health authorities did a 180. They now said that people could protect themselves and others by wearing masks—any and all masks—in public spaces. Their stated rationale for the switch was the possibility of asymptomatic transmission. Owing to the continuing shortage of surgical masks, the CDC recommended “cloth face coverings fashioned from household items or made from common materials at low cost.” Taking their cues from Fauci and the CDC, businesses, schools, universities, and state and local health officials soon fell in line. A policy tool previously regarded within the field of public health as ineffective soon became ubiquitous.
This sequence of events was just one of many times that public health authorities would betray science during the pandemic. Philosophers such as Lee McIntyre emphasize that science is an attitude and approach more so than a domain of knowledge. Good scientists acknowledge uncertainty and convey the limits of what is currently known in their fields. Recognizing that scientific knowledge is provisional, they employ the most rigorous methods available to extend, refine, and even overturn previous understandings. When science is working well, it avoids confirmation bias, bureaucratic CYAs, and politically motivated conclusions.
Both before and after their flip-flop, the nation’s leading public health officials unfortunately demonstrated science at its worst. There was never a strong case in early 2020 for declaring definitively that masks don’t work for COVID. The research the CDC initially relied upon tested only surgical masks, not N95/P2 respirators. In addition, the trials were designed for other respiratory infections, mainly influenza. Some scientists suspected that SARS-CoV-2 had a different means of transmission, and so research on the flu could not automatically be applied to COVID. Meanwhile, there was no rigorous research specifically on COVID to justify the CDC’s new stance on April 3rd, 2020. The agency thus jumped in an unscientific manner from one dogmatic position to another.
Had it actually been “following the science,” the CDC would have transparently communicated its uncertainty at every step. The agency could have informed the public that the best research on other respiratory infections found no benefit from community masking, but the properties of SARS-CoV-2 left open the possibility that the largely cloth and handmade masks available at the time could help in checking its spread. A CDC committed to science would also have worked with other government agencies and private organizations from the first clusters of cases to conduct high-quality RCTs on masking. Such trials would need to be powered with large sample sizes in order to detect modest effects. To this day, they have not funded any RCTs.
Much of the debate over masking has therefore relied on lesser forms of evidence. One approach capitalizes on the policy differences between states. New Jersey implemented the nation’s first statewide mask mandate on April 8th, 2020, and other states soon followed suit. Eleven states never required masks, though, and the other 39 initiated and removed their mandates on different dates. We can therefore compare, for the period when case rates were accurate owing to extensive public testing, the incidence of COVID for states with and without mask mandates. The result? The two groups of states track each other almost perfectly through every surge and decline of cases. If you rely on this quick-and-easy comparison, it’s obvious that community masking failed.
Of course, such a comparison could not be made before the mandates were implemented. It would take some time before the policies could be tracked and evaluated, and nobody knew for sure what the data would show. In the meantime, the credibility of the CDC (and by extension all of public health) was on the line. The agency had already reversed itself once. The pressures were therefore intense for the CDC to find some real-world data to justify its new position.
It did so by trumpeting evidence that any beginning student in research methods would be embarrassed to include in a course assignment. Many people will remember the CDC’s supposedly dispositive case of the Missouri hair salon, which prestigious media outlets dutifully passed along to the public. Two hairdressers with COVID infections wore cloth masks that, according to the CDC, prevented them from transmitting the virus to their patrons. In any other context, we would call this an anecdote. Across tens of thousands of hair salons in America, it could easily happen that two hairdressers with COVID would not pass it to their clientele, regardless of whether they wore masks. The CDC’s “evidence” lacked the most rudimentary aspects of science such as a control group.
Later, the CDC relied on more systematic studies such as a fatally flawed analysis of schools in two Arizona counties. For the last two years, both the CDC and a range of news organizations have pointed to a study conducted in California in 2021. California was still under a mask mandate, and support among the state’s residents for masking was high at that time. The CDC’s study found that wearing cloth, surgical, and N95/KN95 masks reduced COVID rates by 56 percent, 66 percent, and 83 percent, respectively. Its methodology relied on asking people who took a COVID test and knew the result (positive or negative) how often they had worn a mask, and what kind, in the preceding 14 days.
Whether covering voting, church attendance, or food intake, self-reports of this kind are notoriously subject to bias. In the case at hand, people naturally search for reasons to explain their test result, thereby shaping their self-reported mask usage. Someone who tested positive will tend to underestimate their rate of mask wearing by thinking, “I got COVID because I wasn’t masking often enough.” Self-reports from people who tested negative will tend to be biased in the other direction, because they’re thinking, “My mask protected me, and I’m glad I wore it so often.” Notice that the biases will lead to a study finding a systematic relationship between masks and COVID rates even if the masks actually had no benefit.
The CDC and its backers were willing to accept shoddy research based on self-reports so long as it confirmed what they already believed. Whereas masks in the era BC were a nonpartisan intervention that might or might not work and could be studied through the most rigorous scientific methods, they became a morally fraught subject during the pandemic. On the very day the CDC announced its reversal, then-President Donald Trump went off script. He stressed during his press briefing that the CDC’s new guidance was voluntary and that he would not be masking. Over the succeeding months and years, the public followed Trump’s lead and polarized around masks, with liberals and Democrats embracing them at far higher rates than conservatives and Republicans. In blue America, expressing doubts about mask efficacy, or raising concerns about their adverse consequences for relationships and other aspects of physical and mental health, could quickly get you branded as a Trump supporter.
Extensive research in psychology, neuroscience, political science, and other disciplines shows what happens when issues get incorporated into political identities in that fashion. The first casualty is nuance, for people feel pressured to pick a side. Processes of confirmation bias and motivated reason kick into overdrive as people defend their group. Those holding the opposing position get demonized as not just wrong but immoral, and it becomes borderline impossible to engage in rational dialogue based on logic, reason, and evidence. People can even lose their ability to solve math problems when the correct answer would undercut their political commitments.
We can and must demand that public health officials not succumb to these same biases. If you’re going to invoke the mantle of science as the reason why someone should trust you, you have to actually adhere to the best scientific practices, regardless of whose political stances they uphold or undermine. The problem here is that the CDC had painted itself into a corner. By insisting so forcefully that all masks work against COVID, it could not easily back down later. It compounded the error by refusing to fund RCTs that could strengthen the evidence base on which policy recommendations should rest.
Nevertheless, research groups did manage to secure funding to conduct RCTs in two other countries. An RCT in Denmark failed to uncover a statistically significant effect of surgical masks on COVID rates. A later one in Bangladesh found no reliable benefit for the cloth masks that the CDC pronounced as effective in its famous reversal. The Bangladesh study did find a 12 percent reduction in cases for surgical masks, an effect size far smaller than masking advocates would have wanted. However, a series of problems with the study’s design and execution have led other researchers to challenge even the 12 percent figure.
Meanwhile, scientists now know much more about how COVID spreads than they did when the pandemic began. Some scientists at that time suspected a strong role for surface transmission through fomites, more so than happens for influenza. For over a year, many public libraries responded to that threat by quarantining returned books to protect the next reader from their potentially infectious pages. Fomites are now understood to be of only minor importance in spreading COVID.
Some scientists also initially suspected that COVID differed from influenza in having high rates of asymptomatic transmission. If asymptomatic COVID carriers can infect other people, as the CDC stated on April 3rd, 2020, then the same masks that failed to combat influenza could work against the novel coronavirus. Logically speaking, this purported difference between the viruses never made any sense. COVID was well-known from the beginning of the pandemic to cause much higher rates of hospitalization and death than influenza, at least among the unvaccinated (which was everyone at that point). How is it possible that the more lethal virus was also more likely to leave no visible trace among those who contracted it?
Better methods of investigation later found that influenza is at least as likely as COVID to result in people being unaware that they have contracted it. Drawing from recent research, reputable sources now estimate that approximately one-third of all influenza cases are asymptomatic, about the same rate as COVID. Other research eventually confirmed that COVID, like influenza, is transmitted through the air in both droplets and aerosols. With COVID now known to resemble influenza in the means of transmission, RCTs on the latter are obviously applicable to the former.
With that in mind, the Cochrane Library recently published a comprehensive review of the RCTs on non-pharmaceutical interventions (most importantly masking) for the entire class of respiratory infections. What did it find? The report concluded that the current evidence does not support community masking. Before COVID even existed, the New York Times called the Cochrane Library “a respected medical clearinghouse,” “a well-regarded network of independent researchers,” and “the leader in the field” of systematic reviews. One would expect that the newest Cochrane report would therefore be front-page news all over the country.
As it played out, the Cochrane report did not merit a single mention in the New York Times, Washington Post, Wall Street Journal, Los Angeles Times, or USA Today for over three weeks. The first reference in any of those outlets came not through the news sections but rather an opinion column by Bret Stephens. Both Stephens and the Cochrane report soon faced fierce counterarguments. Some of the criticism was fair, such as the difficulty in combining results from RCTs with different designs and populations. The Cochrane Library itself accepted a separate critique that the report covered only mask interventions followed imperfectly by subjects, not the potential benefits of masks per se.
Other responses showed a profound ignorance of evidence-based medicine. One common attack pointed to the laboratory and observational studies supporting masking. By excluding those studies from its purview, the Cochrane authors supposedly engaged in cherry picking. These critics didn’t seem to understand that within evidence-based medicine, focusing on RCTs over weaker studies is a strength, not a weakness. The top of the hierarchy of evidence is a meta-analysis of RCTs, which is precisely what the Cochrane Library offered. Cochrane follows that approach for all of its reports, not just the one on respiratory infections. The same people who previously treated the Cochrane Library as authoritative are being hypocritical in dismissing its conclusions that happen to challenge one of their cherished beliefs.
The report itself, unlike its critics who think they know the truth and proclaim it with utter certainty, follows proper scientific practices in recognizing the limits of current knowledge. The Cochrane authors said the evidence on medical/surgical masks was of only “moderate certainty,” while the data on N95/P2 respirators was “very uncertain.” Rather than declaring the case closed, the Cochrane report called for “large, well-designed RCTs addressing the effectiveness of many of these interventions in multiple settings and populations.” It’s possible that such studies would demonstrate what experts such as Michael Osterholm have said from the beginning: cloth and surgical masks are largely ineffective against COVID, but N95s offer protection so long as they are worn correctly and consistently.
The ball is now firmly in the court of the CDC and other leaders in public health. It’s not too late for them to recommit to science and fulfill the Cochrane request for large-scale RCTs.