Science / Tech
Autism or Encephalitis? My Son’s Misdiagnosis and Our Family’s Season in Hell
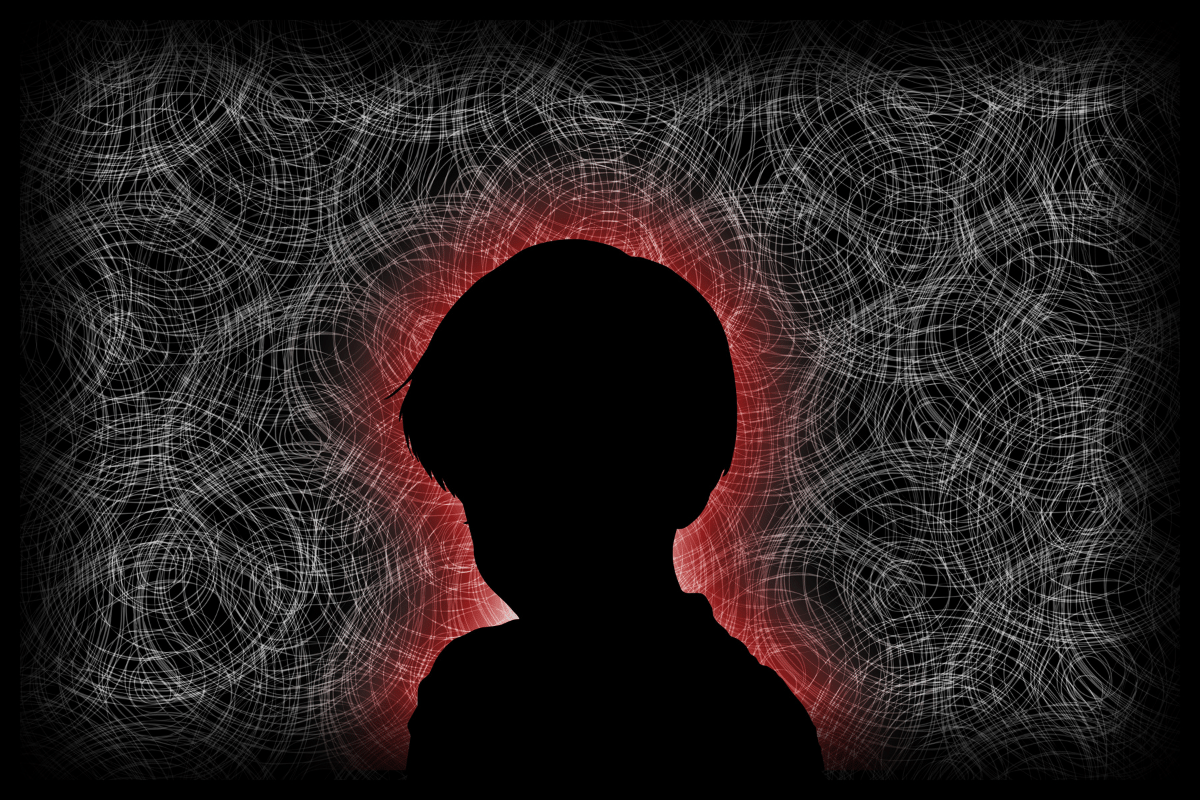
Encephalitis recovery often takes years, not months, and some patients never fully recover.
One night in August 2021, at around 2am, my husband and I were awakened by the sound of laughter coming from our son’s bedroom down the hall. I went in to check on him. Our five-year-old, “Leo,” was awake and running around the room in circles, plowing into toys and furniture in the dark. The expression on his face shocked me. Leo’s eyes were blank; his mouth was twisted into a joker’s grin; his laughter was hysterical and unceasing. He did not respond to my repeated questions, or even notice my presence, but continued in his manic circuit of the room.
Growing desperate, I physically restrained him. For the next three hours, I held Leo in my arms on the bed, while he periodically thrashed, then rested. During his brief periods of rest, he was silent, and I would feel a moment of relief, only for the terrible, braying laughter and thrashing to start again. Mercifully, at dawn he fell asleep soundly. I released my grip and collapsed in exhaustion, weeping. When I woke up later, the room was ablaze with morning light. It was the first day of what would turn out to be our family’s season in hell.
The decline
Leo’s behavior had been deteriorating all summer, maybe even all year, but up until August, it had been so gradual that my husband and I could (just barely) cope. In hindsight, the first indication that something was awry were the sleep disruptions—the vacant expression and manic laughter came later. For many months, bed-time with Leo had been an ordeal. We would put him down at 8pm, and Leo would intermittently call to be let out of his room for hours, usually not falling asleep until midnight. He would often wake up a few hours later, by then 2 or 3am, and either call for us again, or turn his lights on and start playing with toys. This would wake up his baby brother, who would add his shrieks to the general chaos.
Our pediatrician was preoccupied by COVID issues at his practice, and not terribly concerned when we reported our problem. He suggested warm milk and sent us on our way. At that point, we were going on a solid two years of chronic sleep deprivation: first because of our newborn, and then because of Leo. Days and nights blended together like an Impressionist watercolor. Like so many others during the pandemic, my husband and I were juggling working from home with caring for our children. We were also newcomers to LA, with few friends and no family support in town. Bizarrely isolated in suburbia, like the Swiss Family Robinson of the San Fernando Valley, we carried on as best as we could.
Leo grew worse. Sleep disruptions at night began to be followed by tantrums during the day. These grew more frequent and intense. He also began to alternate between periods of hyperactivity and languor. He would stare off into space in our backyard for long periods of time. “He’s communing with nature,” my husband said, but I was uneasy.
His language skills deteriorated. Although normal, even advanced for his age in other respects, Leo had always been a late-talker, so perhaps it took us longer than it should have to realize that he was losing ground cognitively. Looking back, his language skills plateaued around age four-and-a-half. Then all language acquisition halted, and as 2021 progressed, Leo began to lose words. His typical short, ungrammatical sentences changed into two-word sentences; two-word sentences became one-word utterances; one-word utterances became grunts.
He seemed to be either distracted or uncomprehending all the time now—we couldn’t tell which. This was especially pronounced in environments with lots of ambient noise. At a kindergarten meet-and-greet at a park in July, Leo was the only child in the group unable to follow the teacher’s verbal instructions. While the other children ran to a nearby tree as directed, Leo stood rooted to the spot, pathetically copying the teacher’s body-language. The look of fear and confusion on his face was painful to see.
Things came to a head after the night of manic laughter in early August, and our child’s cognitive deterioration went into overdrive. This new symptom, hysterical laughter, marked the dividing line between our life as a normal, if struggling family, to a family in crisis. Leo began having seemingly unprompted laughing episodes more and more frequently, eventually multiple times a day. Sometimes he would laugh for upwards of an hour at a time. This was followed by periods of near catatonia, similar to his spaced-out moments in the backyard earlier that summer. Try as I might to observe this new symptom clinically, the laughter always brought to mind an Edgar Allan Poe poem about demented spirits that “laugh—but smile no more.” It was not the natural laughter of a child. It sounded like the mirthless laughter of the possessed.
A misdiagnosis
The laughter, it would turn out, was the result of a neurological misfire, but we were still weeks away from learning that. Our pediatrician, meanwhile, was persistently steering us in the wrong direction. In the summer of 2020, I had expressed concerns to him about Leo’s poor language skills. He immediately suggested autism, or autism spectrum disorder. (Note: ASD is an umbrella term including autism, as well as a range of mostly less severe related conditions.) He told me that he was leaning toward the latter, even though Leo, at the time, exhibited no other behaviors associated with autism besides language problems. He was affectionate and personable, and communicated well nonverbally. When I said as much, the doctor told me that that’s why it was called a “spectrum,” because children with ASD operated at varying levels of functionality, and some only exhibited one or two typical autism behaviors. Then he rattled off a dozen ASD signs, many of which were so nebulously defined as to be useless, or characteristic of virtually all young children (such as “often ignores parents’ directions”).
I interrupted him to point out that according to his definition, almost everyone on Planet Earth would qualify as a high-functioning autist, which prompted him to politely conclude the appointment. As soon as I got home, I threw his referral list of autism specialists in the trash.
One year and a myriad of bizarre new symptoms later, out of desperation I was now more receptive to the idea that Leo might be autistic. In August 2021, our pediatrician triumphantly diagnosed Leo with the following: 1) autism spectrum disorder; and 2) ADHD (combined type). In writing, he was careful to indicate that this diagnosis was “provisional only” until confirmed by a specialist; however, in our personal interactions for over a year, he had been pushing autism as the main source of Leo’s problems. He gave me the same referral list of autism “experts,” recommending one in particular, a nearby psychologist specializing in the treatment of children with ASD.
He also gave me a list of developmental pediatricians in the area, all specializing in autism or ASD. I called every name on the list, and eventually expanded my search to include any within a three-hour driving radius of our Los Angeles suburb. They were either not taking new patients, or offered me a waitlist of a minimum of nine months. It seemed we were not the only parents in LA who had children corralled into the vast “ASD” category. The demand far exceeded the supply.
To address the (supposed) ADHD, our pediatrician also prescribed Quillivant, the training wheels version of Ritalin. By now Leo’s behavior was so bizarre that I was willing to try almost anything. He was close to nonverbal, and had stopped responding to direct questions. Every day, there was less and less left of Leo, a little boy who used to love putting together 100-piece puzzles, assembling his take-apart toys, watching Octonauts, and swimming in our shabby ’50s era backyard pool. Even his appearance was different. Leo’s eyes were dull and distant. I stopped taking photographs of him because I couldn’t bear to see stills of his facial expression anymore. The new Leo was a child with obviously profound special needs.
We attempted kindergarten, newly medicated on Quillivant. For the rest of my life I will feel guilty for the two weeks I dutifully masked my neurologically impaired, suffering five-year-old, as per the diktats of the Los Angeles United School District (LAUSD). But my husband and I were still clinging to the belief—ridiculous in retrospect—that Leo just had a speech delay, severe ADHD, and possibly ASD.
Kindergarten was an unmitigated disaster. Leo didn’t make it through the first day. He cried, acted erratic, peed his pants, and had to be picked up. The incontinence problem was just one more new symptom to add to the pile. Leo had been potty-trained for years, but suddenly he had forgotten how to use the toilet. We had to put him in pull-ups again.
During Leo’s brief time in kindergarten, his teacher and other school staff did their utmost to stream him into Special Education. Scheduled meetings for testing with the Special Ed teacher were cancelled or delayed at the last minute; Leo was absent because of emergency appointments with his pediatrician.
His teachers and the school nurse were less concerned about Leo’s medical issues, and more concerned that he would not keep his mask on. It was their fixation: almost every communication I had with them was focussed on masking. Masks were (and currently are) mandatory, indoors and outdoors, for all LAUSD students, from kindergarten to 12th Grade. Leo chewed and drooled on every mask, destroying them within minutes. He went through multiple masks a day, and his teacher informed me that when he made tentative attempts to approach other children (by now he was a social pariah), mask hanging low, she steered him away from them for ostensible health and safety reasons. I was aghast at her casual cruelty, but too busy trying to get to the bottom of Leo’s difficulties to put energy into fighting the mask battle just yet.
Despite his doctor’s “provisional” diagnosis, I could not get Leo a mask exemption. His options, according to the LAUSD, were to wear a mask; do online kindergarten (ha); or wear a plastic face-shield, and be removed from class and isolated from the other students, to work one-on-one with a TA in—and I quote the memo—“appropriate personal protective equipment.”
I decided to pull my son out of school for good on the day I was summoned because Leo, once again, had had an “accident.” A harried administrator pointed me to a small room, adjacent to the nurse’s. The nurse—who had previously made it clear that Leo was a simpleton, and I was a poor parent—was nowhere to be seen. Leo was sitting alone in the dark. He was masked, soaked in urine, dazed, and crying. I took him home. Within days, he was admitted to the ER of the Children’s Hospital of Los Angeles (CHLA).
Leo was now in the throes of a complete neurological collapse. He was manic. He was incontinent. He did not know his family members. He could not use a fork or spoon. He could not sit in his chair at meal-times, but would repeatedly crawl under the table. When he ate, he shovelled food into his mouth like an animal, letting it dribble down his face. He no longer enjoyed puzzles. Now, not only could he not complete the simplest one, he would put the pieces in his mouth, and suck on them like a baby.
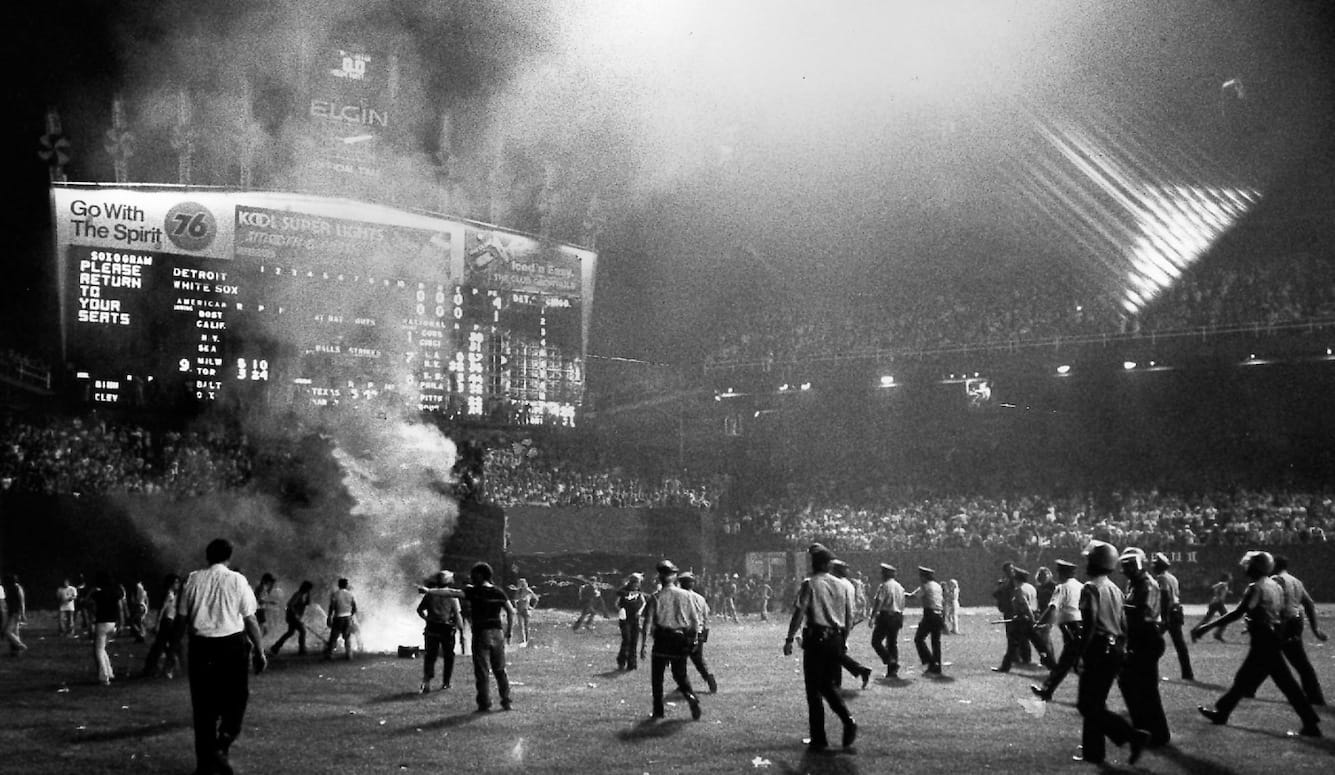
Worst of all, he had started to hallucinate and scream for hours at the thin air. During his worst hallucination episode, he shouted gibberish, pointing frantically at a ceiling fan. When we attempted to soothe him, he ran at us, eyes blazing, hissing and spitting, and tried to fend us off with his little stick-arms. Our house looked and sounded like a scene from Bedlam.
Leo was hospitalized for the better part of two months, while doctors ran every test they could think of that might shed light on his condition. It was a trying time, every day a marathon that my husband and I stumbled through in a haze of physical and spiritual exhaustion. Leo was both there and not there; sometimes calm, and sometimes bewildered and furious like a caged animal. He was administered low doses of sedatives, as needed, with little effect. We often had to hold him down so the nurses could draw blood, and twice Leo bit me. Either my husband or I had to be with Leo constantly in his hospital room, because if he was not always supervised he would hurt himself or break equipment. I rarely had time even to shower in the bathroom a few feet away from his bed.
In the early weeks, we updated our pediatrician by phone. He doggedly clung to his diagnosis of ASD and ADHD, only now adding “probable intellectual disability” to the mix. He was unfailingly polite, but did not listen when we told him repeatedly that Leo had not always been this way. He acted as though my husband and I were in denial about having an autistic and/or special needs child. Without our permission, while we were at the hospital, he gave our contact information to a Utah DNA testing outfit that specialized in diagnosing genetic intellectual disabilities. They began harassing me with calls to my cell phone.
One of Leo’s doctors at CHLA clearly shared our pediatrician’s half-baked assessment, but the vast majority of the physicians there did not. Instead they wisely hedged their bets on his diagnosis until they had proof in the form of positive test results. Leo underwent the following tests (often under general anesthesia, because his unpredictable manic behavior made delicate procedures impossible):
- Two lumbar punctures (a.k.a. “spinal taps”), to draw cerebrospinal fluid;
- Multiple blood tests, including an epilepsy panel DNA test;
- Two MRIs of his brain;
- One MRI of his pelvis;
- Three CT scans;
- Three EEGs.
The first few days of testing all came back negative, while Leo continued to act possessed. The lowest point came after yet another day of fruitless testing. I was feeling demoralized, resting on the cot beside a restless, spaced-out Leo. Our pediatrician’s referral psychologist, the autism “expert,” texted to say my son’s case sounded very much like Childhood Disintegrative Disorder (CDD). She sent a link describing an exceedingly rare and terrifying disorder, often considered a type of regressive, low-functioning autism, that causes children around age four to rapidly lose cognitive skills, and stay more or less frozen at that age mentally for life. I googled horror stories of deterioration and institutionalization. This psychologist had never even examined Leo in person; we had only completed one phone intake interview before he was hospitalized. And yet she was pushing for one of the most serious of all possible diagnoses. I was distraught.

An accurate diagnosis
The situation improved a few days later when we finally had a testing breakthrough. EEG #1 showed that Leo was having seizures. The doctors said it may have been going on for months. At his worst, the EEG was recording two seizures every 45 minutes. In my ignorance, I never suspected this. I was only familiar with the dramatic convulse-on-the-floor-type seizures, properly known as tonic-clonic (formerly grand mal) seizures, not the more subtle focal (or partial) seizures. The neurologists thought it was possible that some of Leo’s mysterious laughing fits were actually rare gelastic or “laughing” seizures, caused by abnormal electrical activity in the brain (in many cases, but not Leo’s, the result of a tumor on the hypothalamus). The post-ictal (or post-seizure) period is often characterized by disorientation and lethargy, which would also explain some of his spacy behavior.
Leo had almost certainly been having multiple undetected seizures behind his mask at school. Instead of helping a terrified child in a post-seizure daze, the teachers and staff covered his breathing-holes with a dirty, wet cloth, and left him alone in a dark room, sobbing.
Never were two parents more delighted to learn their child was having seizures. We had uncovered the first concrete evidence that there was a physical origin to Leo’s suffering. Before then, almost anything was on the table—including autism and the nightmare diagnosis of CDD. Leo’s psychiatry team at CHLA confirmed they could find no evidence of psychiatric disorder, and its chief psychiatrist scoffed at the idea of autism or the ultra-rare CDD. She pointed out that autism does not typically onset suddenly and catastrophically. According to the National Institutes of Health, signs of autism often appear at 12 months or even earlier—not at age five-and-a-half, like Leo.
Leo’s neurologists prescribed Keppra, a standard anti-convulsant that soon stopped his seizures. But we still hadn’t gotten to the bottom of his medical problems. That would take a few more weeks. Eventually, partly through the process of elimination, his neurologists made a final diagnosis: Leo had antibody-negative autoimmune encephalitis (AE).
He was not autistic.
Until then, I had never heard of the disease, which is both relatively rare and serious. It is little known among the general public, though there are an estimated 500,000 cases globally per year. I began educating myself. Encephalitis, put simply, is an inflammation of the brain. There are two broad categories: infectious and autoimmune, the former being more common, and typically more straightforward to treat. Infectious encephalitis is rapid onset and often caused by identifiable viruses, such as West Nile, Herpes Simplex, La Crosse, and many others.
Autoimmune encephalitis, Leo’s sub-type, is more mysterious. In his case, the brain inflammation was not caused by infection, but by his own body producing rogue antibodies that were attacking his brain in error. This can happen in the wake of a previous infection (called post-infectious encephalitis), in response to the presence of a tumour (cancerous or benign), or for reasons unknown. To determine what type of autoimmune encephalitis the patient has, and how to best treat it, doctors test for specific antibodies in the blood or cerebrospinal fluid. This is a relatively new diagnostic advance: the first antibodies associated with the disease, NMDA receptor antibodies, were only discovered in 2007. Since then, 16 other antibodies associated with types of AE have been found.
Leo’s case was further complicated by the fact that none of these antibodies were ever found in his specimens—and to this day, we have never discovered the cause of his illness. This is common: over one-third of encephalitis cases have no known cause. Autoimmune encephalitis is therefore often a diagnosis of exclusion, made partly by ruling out all other options via extensive testing.
Leo immediately embarked on the standard treatments for this disease, some of which were punishing for a very ill five-year-old. He underwent several courses of IV (and oral) steroids to suppress the immune system, and decrease brain inflammation. This was followed by infusions of IV immunoglobulin (IVIG) extracted from donor plasma, to introduce healthy antibodies into the encephalitic patient’s system. The theory is they will bind to the harmful antibodies and neutralize them, among other benefits.
When these treatments did little to improve Leo’s cognitive state, we moved on to plasma exchange (PLEX). This involved hooking him up to a demonic whirring machine which separated his plasma from his blood, discarded it, and replaced it with healthy donor plasma. The purpose was to rid his body of the rogue antibodies floating around, piranha-like, in his plasma. PLEX involved minor surgery, under yet another general, to tunnel a catheter line under the clavicle. In his erratic mental state, Leo often tried to pull the line out of his chest.
When PLEX also yielded few results, his physicians brought out the big guns: Rituximab, a powerful immunosuppressant often given to Lymphoma patients. This was administered in two sessions, two weeks apart. Slowly, in the weeks and months to follow, we began to see improvements in Leo’s general mental clarity. If he had continued to deteriorate, his next treatment might have been cyclophosphamide, a chemotherapy helpful in suppressing the immune system in encephalitis patients.
During the months I spent at Leo’s bedside in the hospital, I occupied myself by voraciously reading any information on encephalitis I could find. There was comparatively little available. The most helpful online resource I found was put out by a UK organization, the Encephalitis Society.
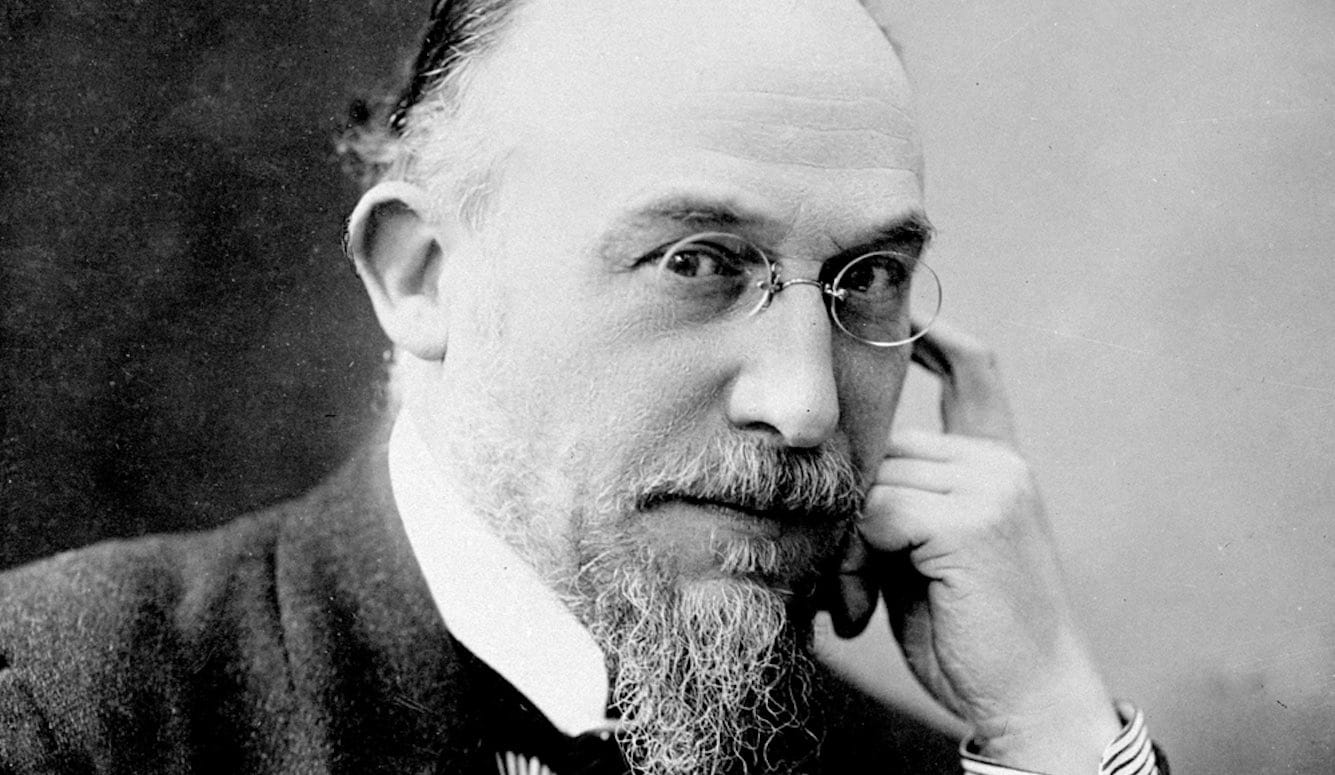
I was most interested in published, first-person patient accounts of encephalitis. By far the best I read was Susannah Cahalan’s engrossing 2012 memoir, Brain on Fire: My Month of Madness. In it, the 24-year-old author recounts her rapid mental and physical deterioration, going from being a sharp-witted fledgling reporter for the New York Post to a drooling, catatonic hospital patient, in under a month. Cahalan suffered from paranoid delusions, hallucinations, and seizures. She was eventually diagnosed with anti-NMDA-receptor autoimmune encephalitis, received the appropriate medical treatment, and made a full recovery. However, for the first few weeks of her illness, doctors believed she was having a mental breakdown. A psychiatrist told her she had mixed episode bipolar disorder; a neurologist suggested “alcohol withdrawal” (though Cahalan was not a heavy drinker).
In adults like Cahalan, encephalitis is often misdiagnosed as schizophrenia, or another psychiatric disorder. I read dozens of patient encephalitis stories on the Encephalitis Society’s webpage, and was struck by how many of the patients were at first misdiagnosed as suffering from mental illness. Some were even wrongfully committed to psychiatric institutions, like Ross Buggins, a 30-year-old IT consultant from Norwich, United Kingdom.
For children with encephalitis, like my son, the disease is often misdiagnosed as autism. To be fair, the two conditions share a number of signs. Both autistic and encephalitic children may have poor communication skills, insomnia, abnormal motor movements, and much more. But critically, encephalitis can be effectively treated. On the other side of the coin, children diagnosed with severe, low-functioning autism (the nonverbal, for example), face a bleak future, and are often eventually institutionalized.
This raises a question: how many children misdiagnosed with autism/ASD actually have autoimmune encephalitis? The neurologists to whom I posed this question at CHLA were, understandably, not willing to speculate. Cahalan ponders the same thing in her memoir, with no clear answers. The brilliant neurologist who diagnosed her case, Dr. Souhel Najjar, estimated that 90 percent of patients suffering from the disease at the time of their treatment (2009) were going undiagnosed. This suggests that the number of cases of “hidden” AE may be high.
According to the UK charity Thinking Autism, there could be “tens of thousands, if not hundreds of thousands” of children and adults misdiagnosed with autism when in fact they have (treatable and usually curable) AE. They argue that the much rarer, supposedly “regressive” cases of autism—when children who have previously met developmental milestones suddenly begin exhibiting “autistic” behaviors—are especially suspect as possible encephalitis cases. (Note: some autism researchers are now arguing that “regressive” autism as classically defined in the field does not truly exist.)
For that matter, what percentage of patients diagnosed with psychiatric disorders are really suffering from autoimmune disorders? Research on the link between psychosis and autoimmune dysregulation is still in its infancy, but growing, as is research linking autoimmune issues to developmental disorders. Intriguingly, a 2021 Frontiers in Psychiatry article, “Autoimmune Encephalitis and Autism Spectrum Disorder,” reviews the literature, and concludes, “AE may either act as a potentially causative agent for ASD, and/or produce symptoms that could easily be mistaken for or misdiagnosed as autism.”
The cost of misdiagnosis and delay in treatment can be catastrophic. Despite medical advances over the past decade, approximately 10 percent of patients with encephalitis still die, often because of brain swelling pressure on the brainstem, the part of the brain that controls vital cardiac and respiratory functions. Once significant brain inflammation has occurred, immediate treatment is critical. When a patient has deteriorated to the point of experiencing seizures and hallucinations, like our son was, the condition is at a crisis-point.
I shudder to think what would have happened to Leo if we had followed our pediatrician’s advice and wasted months treating him for autism spectrum disorder at the clinic of his recommended psychologist. Instead of receiving medical treatment to address the physical origins of his problems, Leo would no doubt have been “treated” with Applied Behavioral Analysis (ABA) therapy, the psychologist’s specialty, per her website and our phone interview. ABA therapy, such as it is, involves repetition and positive reinforcement. For example, some ABA therapists use building block-play to encourage children to communicate. Would Leo have lived if my husband and I had paid thousands of dollars so he could play with blocks for months, instead of treating him with steroids, IVIG, and a powerful immunosuppressant to stop the dangerous swelling of his brain?
As it was, we wasted more than two weeks before we followed our instincts, and rushed Leo to an ER, with the intention of seeing a neurologist immediately. We will never know how much irreparable damage was done to his brain during that time.
Leo was lucky. He had access to all of the resources of one of the best children’s hospitals in the world, and some of the best pediatric neurologists. Leo also had two involved parents who acted as his advocates when he was at his most vulnerable, and who resisted diagnoses with no firm clinical basis. Furthermore, because of my own professional background, I am well aware of the difference between a PhD in Psychology and an MD with a specialization in Psychiatry, when it comes to the expertise required to diagnose neurological conditions. My son needed an experienced neurologist, not a psychologist.
The psychologist who sent me the unprofessional text messages ran a booming autism business. During our phone interview, she told me that many of her clients saw her once or twice a week—for years. Since the 2013 fifth edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5) folded all subcategories of autism, as well as several other related disorders, into one category, ASD, many experts in the field have argued that the definition of autism has become too capacious to be useful. While many autism specialists are professionals and have their patients’ best interests at heart, broadening the definition of autism has created troubling incentives that increase the likelihood of false positives.
During the many sleepless nights when I thought my son was losing his mind, I prayed. I also promised myself that if Leo got better, I would write about our experience, so other parents could prevent their children from suffering. The vast majority of autism cases are not autoimmune encephalitis, but a small percentage are, and that percentage is certainly larger than we realize. Ours is not the only family out there whose child was misdiagnosed as autistic. If you have any suspicion that your child is being misdiagnosed, do not rest until you can see a specialist, preferably a pediatric neurologist with experience diagnosing encephalitis. This is done through standard clinical tests for encephalitis, such as brain scans, blood tests, and lumbar punctures. Mere observation from a psychologist is inadequate. The sudden onset of what appears to be a psychiatric disorder is a red flag. In these instances especially, encephalitis must be considered as a possible diagnosis.
Recovery
Today, Leo is stable and seizure-free. He is in recovery at home. Unfortunately, he is altered. In a 2017 study of long-term neurobehavioral outcomes in autoimmune encephalitis patients, 86 percent reported ongoing neurocognitive symptoms, including emotional lability, fatigue, and short-term memory problems (and 12 percent died). Leo is similar. He is now extremely emotionally volatile, cannot concentrate for long, and has little to no impulse control. Anecdotally, based on my conversations online with other parents of children with encephalitis, we can expect Leo to have continuing behavioral problems in the months and years to come. Some of the parents I communicated with told me their children now struggled in school, and they were worried about their future.
Leo’s language did not magically return. He sees a speech pathologist twice a week, but can still only say a few words. Likewise, his comprehension is now that of a much younger child, possibly an infant. For example, in the first few months of his recovery, when I asked him to clear his dinner plate, he would stare at me blankly. On one occasion, after maybe 10 repetitions of the question, and my acting out of the request, something twigged, and he dumped the dirty plate, utensils and all, into the garbage.
In all probability, Leo has acquired brain injury. This is often called a “hidden disability,” because the person looks ordinary at first glance, but is in fact significantly impaired. In most respects, Leo is now like a one-year-old in a five-year-old’s body. On our walks around the neighborhood, neighbors often smile and say hello to Leo, who rarely responds or makes eye contact. Occasionally he responds with off-putting animal sounds. The neighbors look puzzled. I crack a joke and we quickly pass by.
Encephalitis recovery often takes years, not months, and some patients never fully recover. We know we have a long road ahead. But almost every day Leo shows small signs of improvement. He may still live a normal life. Now we have hope.