COVID-19
The End of Pestilence
The COVID-19 vaccine development experience shows it is possible to produce safe and effective vaccines much faster than previously thought.
Humanity had a vaccine that prevented COVID-19 in January last year. What we did not have was a regulatory system to facilitate rapid assessment of its safety and efficacy or the capacity to manufacture and inoculate at scale.
COVID-19 subsequently caused immense human suffering: over 2.5 million deaths and lockdowns upending the lives of billions. It will be years before most of the world is vaccinated and the global economy recovers.
It need not be this way in future. Humanity is on the cusp of overcoming one of our oldest foes: pestilence. But to achieve this ambitious task it will take a new way of thinking about vaccine development.
Last year there were many who warned of the “risks” of accelerating vaccine development. The Trump Administration’s Operation Warp Speed was criticised for the “potential to cause harm” by loosening safeguards and inciting an antivaxx backlash. If these “go slow” advocates were successful we would still be waiting for vaccines, rather than inoculating millions, saving lives, and on our way to ending this dreadful pandemic.
“It’s just like people breaking the five-minute mile or the four-minute mile and things like that,” Harvard epidemiologist, immunologist, and physician Michael Mina explains:
People think, Oh, you’ll never do faster than that. It’s like, well, actually you can break it by leaps and bounds more. You just have to think differently. So many times we hear people say things like the vaccine trials could never have been sped up any faster. Well, yes, it could. Where there’s a will, there’s a way.
The COVID-19 vaccine development experience shows it is possible to produce safe and effective vaccines much faster than previously thought. But why should 11 months be the best we can muster? The challenge now is to figure out how the entire process can go even faster while maintaining, or even improving, safety.
Learning from COVID-19 vaccine development
In the past, vaccine development took 10 to 15 years. There was the slow grind of writing and rewriting grant applications, researching and developing the vaccine, preclinical animal testing, waiting for trial approvals, recruiting volunteers, three stages of clinical trials, negotiating with pharmaceutical companies, and then waiting for regulators to get around to looking at findings for approval before manufacturing can even begin—let alone distribution and inoculation.
These steps are normally undertaken sequentially with long delays between each stage. This is an expensive and unappealing process, especially considering the low profitability of vaccines (they make up just a few percent of the trillion dollar global pharmaceutical industry).
Historically, vaccines have often not arrived till after the bulk of the damage from an infectious disease. COVID-19 changes that. Just over a year after the emergence of virus we already have an extraordinary range of safe and effective vaccines: mRNA vaccines from BioNTech/Pfizer (95 percent effective) and Moderna (94 percent), the viral vector vaccines from Oxford/AstraZeneca (82.4 percent) and Johnson & Johnson (85 percent), as well as a protein vaccine from Novavax (89.3 percent).
These vaccines were rapidly developed because of previous research, new technologies, and a whole-of-society focus on combating the pandemic.
Scientists knew, from earlier coronaviruses research, that the spike protein on the surface of the virus that causes COVID-19 would be an ideal target for a vaccine. They had also been working on “vaccine platforms”: pre-existing vaccine technology that can be rapidly adapted to a new viral threat. So when the COVID-19 genetic code was released last January they could immediately plug the spike protein into their platforms to create new vaccines.
ChAdOx1, developed by Oxford University’s Jenner Institute, is an exemplar “vaccine platform.” It uses a harmless chimpanzee adenovirus (the vector) that contains the genetic information for our cells to make the spike protein from the COVID-19 virus—our immune system responds by building antibodies to defend against the virus. ChAdOx1 had previously been adapted and tested in humans and mice for the flu, Zika, and prostate cancer.
ChAdOx1 was shown in 2017 to produce neutralising antibodies against Middle East respiratory syndrome (MERS) coronavirus in mice, and later in humans, using the MERS spike protein. So when COVID-19 came along it was a relatively straightforward task to update ChAdOx1 to reflect the latest threat. Johnson & Johnson’s and Russia’s Sputnik V are also viral vector vaccines that use an inactivated adenovirus to deliver the spike protein.
Moderna and BioNTech/Pfizer developed synthetic messenger RNA (mRNA) vaccine platforms. mRNA vaccines contain a tiny genetic code that teaches human cells how to make a protein—the spike protein in the case of COVID-19—to trigger an immune response. Moderna’s COVID-19 vaccine was developed within just 48 hours of the sequencing of the virus last January and the first doses were manufactured within a month for a phase 1 trial.
The mRNA vaccines represent a gigantic scientific leap. Before COVID-19, no mRNA vaccine or drug had been approved by regulators and many scientists were sceptical. Now the technology could be used to tackle cancer, HIV, and rare diseases. Already mRNA technology has been used to develop the first vaccine to fully immunise against malaria. Malaria is one of the most deadly diseases in human history: it was responsible for up to 300 million deaths in the 20th century and is continuing to kill around half a million people per year.
Importantly, mRNA vaccines can be more rapidly developed and produced at scale than other vaccines because they use a synthetic, computer-based process. That is, scientists can effectively print the necessary genetic code, rather than relying on a biological process involving cell cultures or fermentation like traditional vaccines. This also makes it much safer and more precise than previous vaccine techniques.
In addition to previous research and emerging technologies, the COVID-19 vaccines were supported by plentiful public and private investment. This included substantial advanced purchase orders and manufacturing investment. This allowed the companies to construct factories and manufacture vaccines before the completion of phase 3 trials without the risk of losing billions.
Moderna received $2.48 billion from Operation Warp Speed for development and production of 100 million doses. Pfizer invested $2 billion into the project. They refused to take Operation Warp Speed cash for vaccine development to “liberate” their scientists from any bureaucracy. They did, however, accept a $1.95 billion US government contract for 100 million, and advanced orders from other governments.
Previously slow regulators also took a timely approach: rapidly approving trials and allowing trial phases to be undertaken simultaneously. Moderna began with humans rather than animals. Oxford combined phase 1 and phase 2 while Pfizer/BioNTech combined phase 2 and phase 3. Additionally, rather than just taking a look at the end, regulators undertook “rolling reviews” of safety, manufacturing and effectiveness. This meant that when phase 3 trial results began to be released last November regulators already had substantial knowledge of the vaccines and millions of doses were being manufactured. Consequently, immensely effective vaccines could be rapidly developed, produced, and approved without sacrificing safety.
More and updated vaccines to tackle COVID-19
Now that we have effective vaccines the challenge is to inoculate the world. So far success is highly mixed: 54 percent of Israelis, 30 percent of Brits, and 15 percent of Americans have received at least one jab. The European Union has vaccinated less than five percent of her population. Asia has reached less than two percent. Africa has done less than 0.3 percent.
In order to match global demand there is an urgent need to accelerate the development of additional COVID-19 vaccines, as well as expand the approval, manufacturing, and distribution of existing vaccines. One proposal is to place vaccine patents into the public domain for anyone to produce. But even if this was done it would not lead to increased vaccine production, which is a complicated and expensive process requiring specialised knowledge. It also risks less investment in vaccine development in the future. Rather, governments should pay more for doses and invest in additional manufacturing capacity. They should also be transparent about availability and learn from Israel’s effective distribution and zero wastage.
The global vaccination programme is also undermined by the emergence of COVID-19 mutations. The South African (B.1.351) and Brazilian (P.1) variants contain a modification to the spike protein that makes the existing vaccines less effective, including BioNTech/Pfizer, Moderna, Novavax, and Oxford. This is only just the beginning. This danger of vaccine-resistant mutations will continue to grow as parts of populations are vaccinated while community transmission continues. This is because a vaccine-resistant mutation among the unvaccinated population, that would be irrelevant if nobody was vaccinated, can now easily spread among the vaccinated population.
The danger of mutations is increased by the fact that nine-in-10 people in poor countries will not receive a COVID-19 vaccine this year. While it may be morally justifiable for developed countries that have invested huge amounts in vaccine development to prioritise their citizens this does not absolve responsibility to support developing nations. If nothing else there is the self-interested need to avoid the risk of foreign vaccine-resistant mutations being imported.
Thankfully, virus variants undermining vaccines is not a new challenge. The flu is constantly mutating, requiring global monitoring and an annual vaccine update—a process that dates back to the 1950s. Twice a year—in February for the Northern Hemisphere’s winter and September for the Southern Hampshire—the World Health Organisation convenes a meeting to assess which influenza strains are most likely to spread and cause illness. They recommend a flu vaccine that typically includes two influenza A (H1N1 and H3N2) and one or two influenza B strains.
Manufacturers then update their vaccines to reflect the latest strains. The flu vaccine is typically manufactured using fertilized hen’s eggs to incubate the virus, which is then extracted, inactivated and purified. Importantly, regulators, in the knowledge the existing flu vaccine manufacturing techniques are safe and effective from earlier trials, do not require the updated vaccines to be put through randomised controlled trials (RCT).
The Centres for Disease Control (CDC) states randomised control trials for the flu vaccine are unethical because it would require denying a potentially life-saving vaccine to a “control” group to compare outcomes with a vaccinated group. The potential benefits of an RCT, in confirming safety efficacy, are outweighed by the potential costs to human life when we already know a vaccine to be safe.
Instead, each batch is quality tested by regulators before it is filled into glass bottles and distributed. They also use observational studies, witnessing different outcomes for those who choose to get vaccinated and those who do not, and non-randomised studies that test an individual’s immune response after a vaccine. This process means humanity can benefit each year from flu vaccines, rather than waiting years each time.
If we are to have any hope in combating COVID-19 variants without repeated lockdowns and limits on global travel, it will be necessary to apply the same regulatory approach to updated COVID-19 vaccines. Now that COVID-19 has spread so widely it will probably turn endemic, constantly mutating and requiring annual immunisation like the flu.
The process should be straightforward: a vaccine-resistant variant is identified by genomic sequencing, the existing mRNA, vector and protein vaccines are updated and immediately produced for small-scale testing to recheck safety and efficacy. They are then mass produced under the usual regulatory supervision and the public is provided with “booster” inoculations. They could even be provided simultaneously with the annual flu shot.
Moderna have already manufactured an updated version of their vaccine to tackle the South African strain. It will shortly be undergoing human study. This entire process of updating a vaccine, according to Britain’s vaccine minister Nadhim Zahawi, could take as little as “30 to 40 days.” In the US, the Food and Drug Administration (FDA) have released updated guidance stating that existing vaccines updated for new variants will not require randomized control trails. They can instead be tested in small trials to confirm safety and immune system response.
An alternative is the development of a “universal vaccine” that targets the core of the coronavirus which is less likely to mutate. There is even a nasal spray vaccine, currently being tested in animals, that takes this approach. Scientists are also hopeful of developing a “pancoronavirus vaccine” that could work against all coronaviruses in future. Early experiments involving mice indicate cross-reactive immune responses to vaccines which contain multiple coronaviruses. The side benefit of which could be to reduce the severity of the common cold, many of which are a coronavirus.
How to accelerate new vaccine development
There remains a significant risk of future pandemics from animals, which host thousands of viruses that could jump to humans, and bioterrorism. Frighteningly, the next pandemic could spread faster or be more deadly than even COVID-19. The development of “plug and play” vaccine platforms raises the opportunity to prevent future pandemics and important ethical questions for regulators.
Ending pestilence: A seven step plan
- Research viral threats, identifying families of viruses most likely to produce pandemics;
- Develop vaccines in response to those viruses;
- Test vaccines in animals and phase 1 (safety) and phase 2 (efficacy) human trials;
- Invest in manufacturing capacity for two billion doses per year;
- Develop logistics for distribution and rapid mass vaccination programmes;
- Prepare challenge trials for new pathogens, in which volunteers are given a vaccine and exposed to the virus to test safety and efficacy; and
- Reform regulatory processes to enable for faster approval.
One approach, proposed by Florian Krammer of the Icahn School of Medicine at Mount Sinai, is for the investment in the development of vaccines for 50–100 viruses with the highest likelihood becoming pandemics. These would be subjected to phase 1 (safety) and phase 2 (efficacy) testing. These individuals would be monitored for decades, allowing for the assessment of the protective longevity and increasing confidence in safety. Krammer claims this preparation would cost around US$1-3 billion in total—practically nothing compared to the trillions the COVID-19 pandemic has cost the global economy. Krammer envisages that when a new virus emerges the closest existing vaccine is chosen to develop a new vaccine. This would then immediately be put into a phase 3, randomised controlled trial involving thousands of people.

Even more controversially, it may not be necessary to undertake randomised controlled trials on each new use of an existing vaccine platform—in the same fashion that trials which deny access to a vaccine are unethical for influenza or new COVID-19 strains. A randomised control trial should only be used when “there is genuine uncertainty about whether an untested treatment has benefits or risks that exceed those of conventional care.” The justification breaks down when a treatment is known to be safe and effective while conventional care is known to have a substantial risk of death. If previous research and initial smaller trials show a vaccine to be safe and effective in the face of a pandemic which could kill millions, waiting many months for a randomised control trial would be unethical.
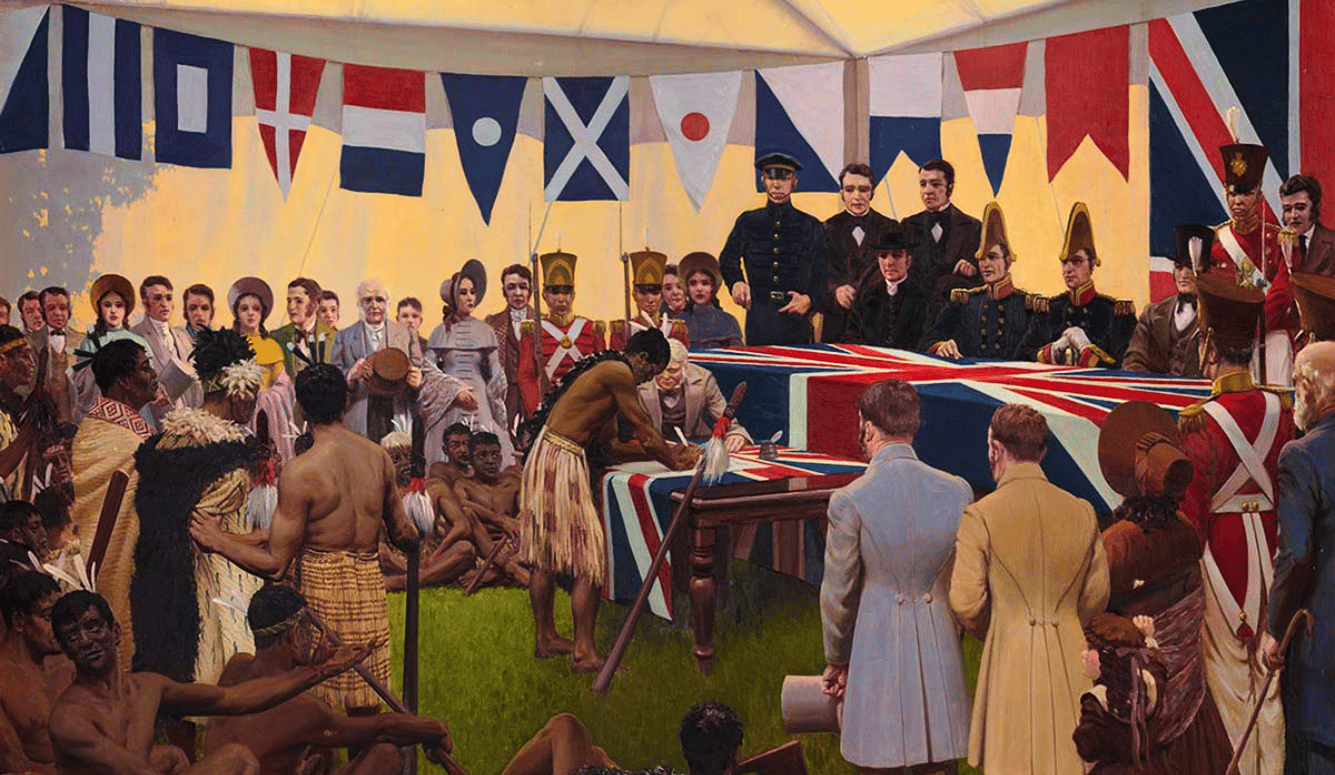
An alternative approach is human challenge trials: exposing individuals to a virus (the challenge), in a carefully controlled environment, to learn how they respond to a treatment. The first such trials were used by vaccine pioneer Edward Jenner in 1796, who exposed an eight year old to live cowpox virus. They have also been used to develop vaccines and treatments for typhoid, cholera, and malaria. Challenge trials provide reliable and accurate results while involving few individuals and costing substantially less than a randomised control trial. They can also be undertaken before a virus is circulating in the community.
The UK recently began the first challenge trial for COVID-19, involving healthy 18-30 year olds. This came after lobbying by 1Day Sooner, who have registered over 38,500 volunteers in 165 countries. The beginning of this study is less miraculous than it took so long. If scientists had begun human challenge trials last February we could have known the safety and effectiveness of the vaccines many months earlier, speeding up regulatory approval, manufacturing, and distribution and potentially saving hundreds of thousands of lives.
In addition to development and trails, there will also need to be substantial manufacturing capacity that is either idle or capable of being repurposed. This will need to be matched by a global logistics effort and vaccination centres to get jabs into people’s arms. We will also need a system of constant global vigilance to identify new viral threats, a willingness to use border controls, and systems for effective testing and tracing prior to a vaccine.
Finally, regulators will need to update their approach to reflect the latest technology. We have seen throughout the last year how agencies like the US’ Centers for Disease Control and Prevention and Public Health England severely hampered the expansion of testing capacity at the start of the pandemic, which contributed to uncontrolled outbreaks. On the other hand, the fast-moving UK Medicines and Healthcare products Regulatory Agency (MHRA) meant that the British were the first in the world to access the BioNTech/Pfizer and Oxford/AstraZeneca vaccines.
Medical regulators should recognise the immense safety and efficacy of the new vaccine platforms as well as being open to challenge trials. No corners should ever be cut, but nor should a lifesaving vaccine be restricted because of unnecessary bureaucracy. For instance, it is unnecessary for regulatory agencies in smaller countries to duplicate the work of their equivalents in larger countries where vaccine trials are authorised and undertaken. They should, instead, recognise approvals by the likes of the UK, EU, and US regulators.
The final challenge will be persuading the public to take a vaccine. There will no doubt be substantial and genuine hesitancy about a rapidly developed vaccine, as we are already seeing in response to the COVID-19 vaccines. There are risks associated with speeding up vaccine development. These must be taken seriously and addressed by maintaining the highest of standards and carefully communicating with the public about the potential risks and benefits.
For instance, the constant reference to the Cutter incident, which resulted in 200 children with paralysis and 10 children dying, is unhelpful. This was the result of a manufacturing fault, which resulted in a polio virus not being properly inactivated. The latest vaccine technologies do not contain inactivated virus. This, along with improved safety and batch testing, makes them much safer.
* * *
A future pandemic will be a policy failure, a choice to not harness the latest technologies, invest in vaccines, as well as prepare systems for rapid regulatory approval.
Someday humanity may just look back on COVID-19 as a turning point. We had the vaccines the entire time. We learnt from that experience that speed is a virtue during a deadly global pandemic. We used new technologies to speed up vaccine development: improving preparedness by investing in vaccine platforms, manufacturing and distribution capacity and regulatory speed by embracing challenge trails. We managed to consign pandemics to the history books.
After a miserable year, we have the means to overcome one of humanity’s biggest menaces. The challenge is to make that a reality.