Bioethics
Human Challenge Trials—A Coronavirus Taboo
If we can overcome the taboos surrounding HCTs, they can become a game changer in combating the coronavirus and limiting its ruinous effects on countless lives.

The idea is as simple as it is apparently repulsive: allow human challenge trials (HCTs) under which “low risk” and healthy young adult volunteers in double-blind studies would be given trial vaccines (or a placebo) and then intentionally exposed to the novel coronavirus. This would accelerate the assessment of the trial vaccine’s safety and efficacy and more generally expand our understanding of this virus in a controlled setting.
According to the World Health Organization (WHO), more than 70 vaccines are currently under development, five of which are already moving to clinical trials. Notwithstanding these Herculean efforts, the earliest we can realistically expect a readily available vaccine is in 12 to 18 months. This is in large part due to constraints imposed by traditional vaccine validation methods, which rely on large test groups and chance exposure to the virus by participants to assess the vaccine’s safety and efficacy. HCTs, using a relatively small low-risk group of volunteer participants, could potentially accelerate the release of a safe and effective vaccine by many months.
While conducting coronavirus HCTs raises various ethical questions, a compelling case can be made for their use based on the current data. By speeding up the release of a safe and effective vaccine, HCTs could save hundreds of thousands of lives or more, globally. Additionally, this could save trillions of dollars of unnecessary damage to the US and global economies, and spare millions (or even billions) of people untold despair and misery.
On March 15th, 2020, Dr. Anthony Fauci, the director of the US National Institute for Allergy and Infectious Diseases declared on national television that, in the fight against the novel coronavirus, “everything is on the table.” Until recently, however, absent scattered voices and academic papers, consideration of HCTs has been treated as a taboo subject by our public health officials and political leaders. To date, neither the Trump administration nor the US Food and Drug Administration (FDA) or Centers for Disease Control and Prevention (CDC) has provided any definitive public guidance or position on HCTs with regard to the coronavirus. Why is this potentially important tool such a taboo topic?
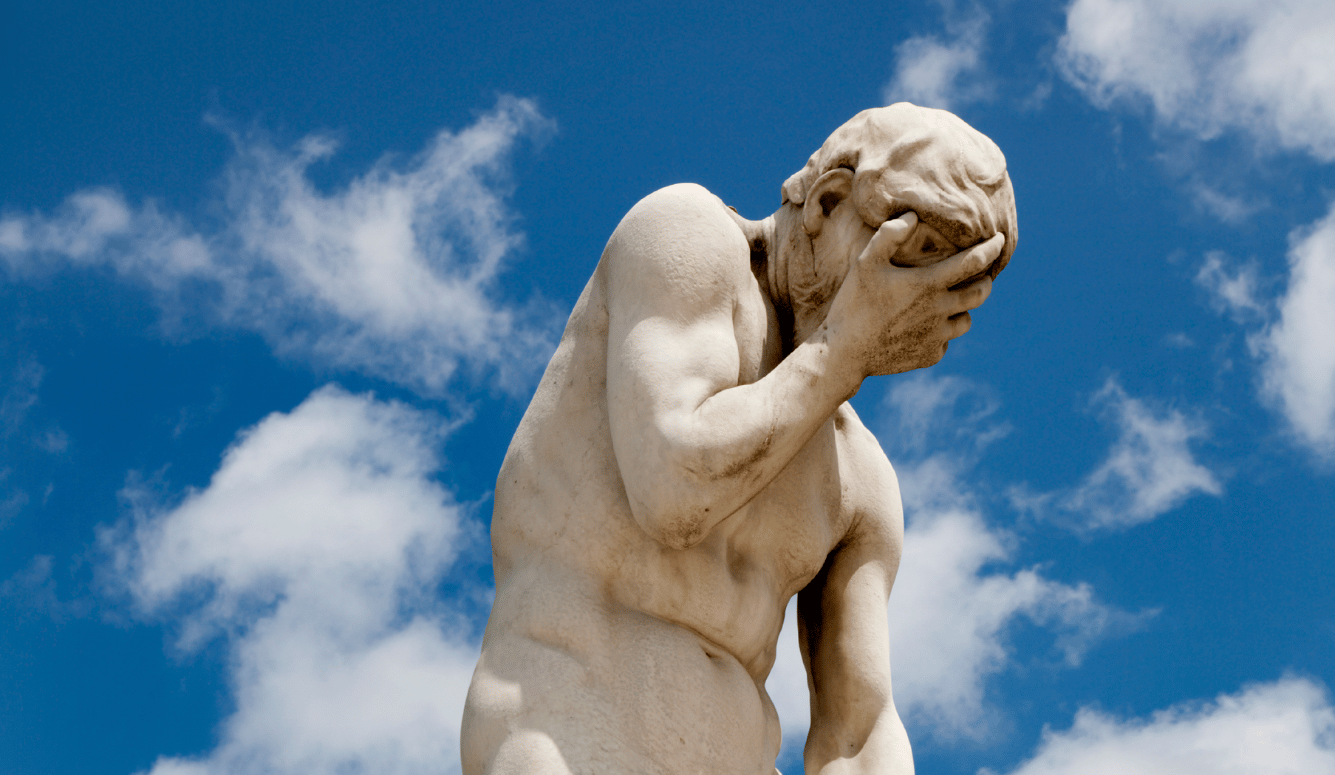
In my casual conversations with friends, family, and colleagues, the consistent reaction to the idea of HCTs has been first, an awkward silence, quickly followed by a rejection of the idea as either immoral, impractical, or both. Then—if I am able to continue the conversation long enough to walk them through the current data—a reluctant “maybe,” but usually with a lingering hint of distaste and suspicion, as if I had somehow manipulated them into an unpalatable and unwanted conclusion that violates their better judgment.
On the one hand, I find this instinctive revulsion at the idea of HCTs wholly understandable (and perhaps even laudable)—after all, even if the participants are all “volunteers,” HCTs sanction the deliberate exposure of otherwise healthy individuals to potentially dangerous (and in the case of this coronavirus, potentially deadly) experimentation. As one friend bluntly objected, “It all sounds a bit too Dr. Mengele for me.” One needn’t be a Nazi to perpetrate such atrocities. American 20th century history offers its own bioethical horrors, from the infamous 1932 Tuskegee Study to many lesser known tragedies and abuses of HCT and human experimentation in the name of science.
On the other hand, as individuals and as societies, we effectively conduct these types of human “experiments” on a daily basis (knowingly and unknowingly) by balancing risks, including the risk of death, against perceived benefits of various courses of action or inaction. When the US Environmental Protection Agency (EPA) sets air pollution and particulate standards, it explicitly calculates the number of expected annual deaths that will occur at various levels of air quality. The EPA then agrees a standard that accepts some level of expected air-pollution-related deaths based on this risk/benefit analysis.
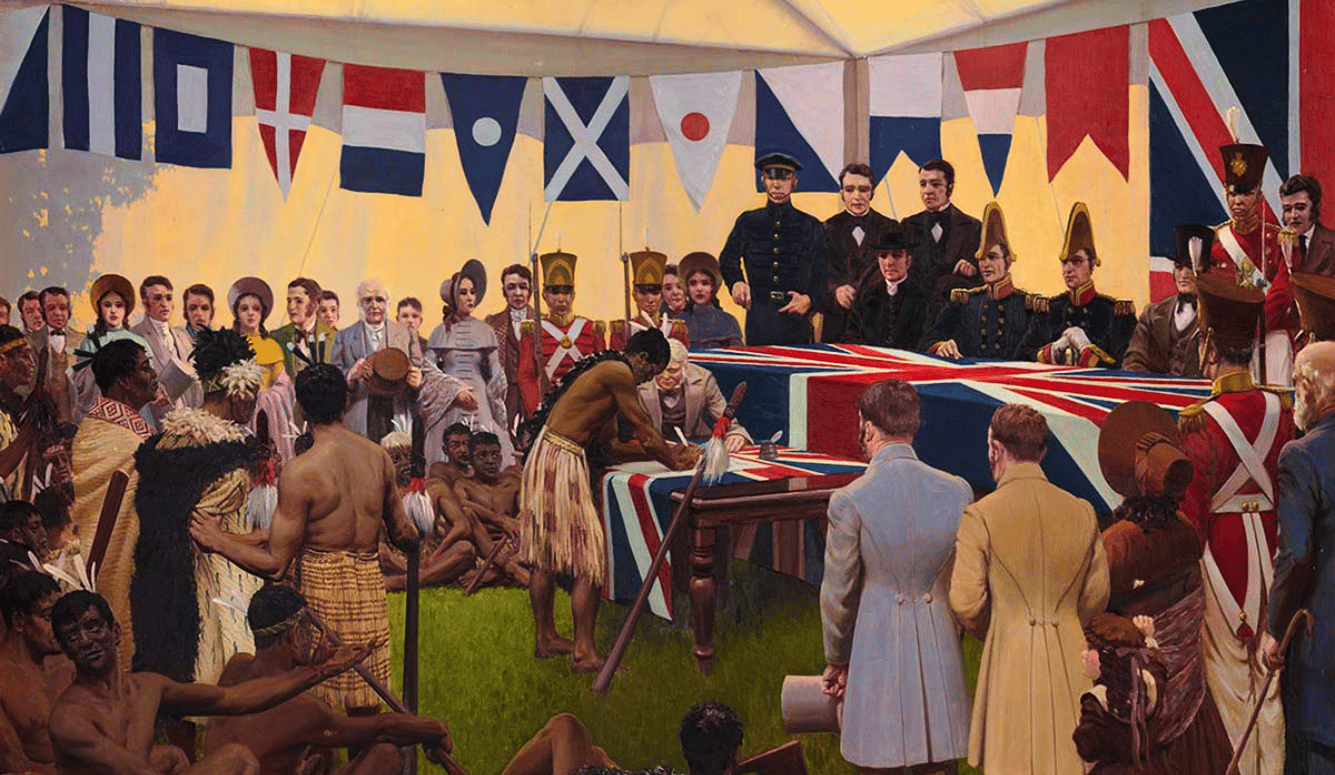
HCTs are not a new idea; a WHO report in 2016 noted that “human challenge studies have been conducted over hundreds of years and have contributed vital scientific knowledge that has led to advances in the development of drugs and vaccines.” In past HCTs, doctors and scientists have infected volunteers with diseases that include influenzas, malaria, dengue, typhoid, and cholera. While rare today, even under established medical ethics guidelines and protocols, these human clinical experiments still can be deadly. In 2001, a healthy 24-year-old died as a result of her participation in a study at the Johns Hopkins Asthma and Allergy Center. So, caution and thorough consideration of any HCT are essential to ensure that the relevant risks/benefits are adequately understood. These must be assessed by the appropriate scientific and bioethicist review board and by the volunteer participants themselves, in keeping with the foremost Hippocratic principle of medicine: “First, do no harm.”
By its very nature, COVID-19 presents a unique opportunity to use HCTs to accelerate the development of a safe and effective vaccine. COVID-19 has many bad attributes, but one potentially useful attribute is that the infection fatality rate (IFR) for the relatively young (20 to 39 years old) and healthy population segment is comparatively low. This characteristic allows for the identification of a group of healthy young volunteers to be part of one or more HCTs. In addition to potentially significantly shortening the time required to develop and validate a safe and effective vaccine, use of HCT volunteers could also quickly expand our basic understanding of the virus, and potentially answer important questions such as: Does the amount of initial viral exposure affect the severity of the illness? Can asymptomatic carriers transmit the disease? Are individuals with COVID-19 antibodies protected from reinfection? Do certain medications provide prophylactic protection against infection? These citizen volunteers, along with all the frontline and other essential personnel, could make a historic and critical contribution to vanquishing the threat of COVID-19.
The evidence in support of adding HCTs to our coronavirus toolkit has grown in recent weeks. New data gleaned from preliminary antibody tests indicates that the spread of the virus may have been significantly more widespread than initially believed. And it looks increasingly certain that the risk of hospitalization and death from COVID-19 is relatively low (though by no means nonexistent) for healthy young adults aged between 20 and 39. At the end of April 2020, Governor Cuomo announced that antibody testing of 3,000 New York State citizens (updated as of April 27th, 2020) indicated that 14.9 percent of the general population in New York State and 24.7 percent of the NYC residents had already contracted COVID-19. New York State has a total population of roughly 20 million. Of these, approximately 5.3 million are between the ages of 20 and 39. If 14.9 percent of this group has developed COVID-19 antibodies, it would imply that 789,700 New Yorkers in the 20 to 39 age bracket have already been infected.
As of April 24th, 2020, there had been 304 reported COVID-19 deaths in this age cohort. Of these 304 deaths, 194 had one or more identified underlying health conditions (hypertension, diabetes, obesity, renal failure, cancer, etc.), leaving 114 deaths in the 20–39 age range that were not associated with an underlying comorbidity. If the antibody sampling percentages are accurate, that would mean that the morbidity/IFR for this 20 to 39 age and health cohort is roughly 0.014 percent or 1.4 deaths for every 10,000 infections. In other words, the survival rate in this cohort is 99.986 percent. Similarly, a study of excess deaths in Italy reports an IFR of 0.017 percent in those aged between 20 and 41 years old (without regard to the presence of any comorbidities). In an HCT, we would therefore expect a similar (or lower) risk of death amongst the volunteers in the same age and health cohort who actually contracted COVID-19.
While any coronavirus deaths are tragic, 1.4 deaths per 10,000 is remarkably low. For comparison, the fatality rate in the US for a kidney donor is roughly three deaths per 10,000 (more than double the estimated risk of a HCT coronavirus volunteer)—a fatality rate that both society, from an ethical cost/benefit standpoint, and each individual kidney donor, from a personal safety standpoint, willingly accept. And coronavirus HCTs are arguably supported by even more compelling justifications in terms of the total potential number of lives saved and other societal benefits. Similarly, the 0.014 percent fatality risk for coronavirus volunteers even compares favorably with the job-related fatality risk faced each year in many professions. According to US Department of Labor statistics, fishermen, loggers, air pilots, roofers, trash haulers, steel and construction workers, truck drivers, ranchers, farmers and other agricultural workers, lawn and groundskeepers, and many other professions all have a higher risk of death from their jobs each year than would a HCT coronavirus volunteer.
If we expected, say, 1,000 HCT coronavirus volunteers to contract the virus in HCTs, we would, statistically, not expect to have even one volunteer (out of the 1,000) die as result of the trial because the expected IFR would be 0.14 deaths per 1,000 (an average of one death per 7,000+ infected HCT volunteers). Obviously, to the extent scientists and doctors can design the relevant studies to have fewer than 1,000 people actually contract the virus, this risk of having even one death would become even more remote. In the absence of a vaccine, a significant percentage of HCT coronavirus volunteers (particularly those living in large, dense urban environments) would likely contract the virus over time in any case, but with potentially worse outcomes—they would become infected without the high level of supervision, monitoring, and potentially without the prompt and preferential medical treatment that would presumably be made available to them as HCT volunteers (including preferential access to any promising novel treatment therapies). And, to the extent that the severity of the reaction to the virus is dependent on the initial exposure dosage, the HCTs could, by limiting the exposure levels, limit the potential of a volunteer to become severely affected until the vaccine’s efficacy can be confirmed.
In addition, hopefully many of the trial vaccines administered will turn out to be safe and efficacious, so a large number of the 1,000 HCT volunteers would not actually become infected, leaving only a small percentage of volunteers (mostly those given a placebo) who would actually contract COVID-19 and be at risk. It may also be possible to further circumscribe the applicant pool by accepting only 20 to 30-year-olds and/or by screening for hidden comorbidities or genetic vulnerabilities in order to further reduce the risk to volunteers. Finally, by their very nature, HCTs offer the opportunity to test vaccines on smaller sample sizes. Non-HCTs require many more people to be inoculated, so HCTs would provide additional protection if it later turned out that the vaccine administered was for some reason dangerous or unsafe. Given the current data indicating that it is statistically unlikely that even one coronavirus volunteer would die as a result of the HCT, and the potential of HCTs to reduce the time required to create a safe and effective vaccine, thereby saving thousands of lives and trillions in economic carnage, HCTs should be given close consideration and should be part of an open discussion and debate among public health officials, political leaders, the scientific community, and the general public.
If the Trump administration and the public health officials at the FDA and CDC were to conclude that coronavirus HCTs are a worthwhile endeavor in the battle against the coronavirus, an important question remains: Would sufficient volunteers actually come forward to participate in such trials? We will not know the answer to that question for certain until we ask, but I suspect that properly positioned, many individuals would willingly volunteer, just as many volunteered to help out (or enlisted in the military) after 9/11 or volunteer every day to donate a kidney or engage in other acts of altruism. In fact, we have positive indications from a non-profit (1 Day Sooner) that, as of May 1st, 2020, nearly 9,000 individuals from 52 countries had already expressed a willingness to take part in coronavirus HCTs.
The chance to play an important role in conquering this disease (even at some level of personal risk) would, I suspect, be attractive to many. An opportunity for service, purpose, and even self-sacrifice, especially at a time when most of us are being told that the best—and frankly only—thing we can do is to withdraw and self-isolate at home, might resonate with the public. This willingness of individuals to volunteer for HCTs also comports with the results of numerous sociological and management studies confirming that humans seek (and highly value) having purpose and meaning in our lives—often more than financial and other material rewards. An appeal to individuals whose primary motive is to help the world defeat this virus is likely to be sufficient to secure a sufficient number of qualifying volunteers, without requiring any large financial incentives, besides costs and expenses.
If we can overcome the taboos surrounding HCTs, they can become a game changer in combating the coronavirus and limiting its ruinous effects on countless lives. A recent paper by a Harvard epidemiologist, a Rutgers bioethicist, and a London School of Hygiene & Tropical Medicine epidemiologist sets forth proposed protocols for how a coronavirus vaccine HCT might be conducted. In the US, meanwhile, some lawmakers are beginning to look at the issue. Recently, 35 bipartisan members of Congress signed a letter to the FDA and US Department of Health and Human Service in support of coronavirus HCTs. Time, however, is of the essence.