recent
Inside the Woke Actors Studio: How I Trained Future Doctors to Police Their Pronouns
But pulling off the kind of manipulative narcissism that privileges ideological dogma over real community health needs—that’s the mark of a true pro.

I’ve always considered myself a collector of interesting experiences. Perhaps to my detriment, my résumé looks more like a roster of Whose Line Is It Anyway sketches than a sequence of interrelated experiences leading up to a stable professional life. Never-a-dull-moment has been the goal, and most moments have remained gratifyingly un-dull.
So when a local medical school asked me to serve as a simulated patient for their training sessions, I jumped at it. I had absolutely no acting experience, and most of my medical knowledge is on the level of Dr. Phil. But maybe this is how stars are born. You’re Pertussis Patient #3—until a blotto Bradley Cooper walks into the ER and overhears your beautiful coughing fit.
Some of my fellow med-school thespians are, like me, simple university students looking to make a buck. But some are actors manqués who’d apparently been doing this for decades: elderly men and women who put on makeup, affect accents, and invent their own evocative pseudonyms and back stories that go way beyond the simple patient scripts assigned to us.
Readers may recall The Burning, a ninth-season Seinfeld episode in which Kramer and his friend Mickey become simulated patients at Mount Sinai hospital. Mickey is thrilled when he learns he’s been assigned bacterial meningitis, which he calls the Hamlet of diseases. (“Severe pain, nausea, delusions…It’s got everything.”). Meanwhile, hilarity ensues when Kramer hams it up in his effort to act out gonorrhoea. (“Our eyes met across the crowded hat store. I, a customer, and she a coquettish haberdasher…I burned for her, much like the burning during urination that I would experience soon afterwards.”)
Unfortunately, the real world of fake-patient acting isn’t fun at all, since—well, since you’re in a hospital surrounded by people who are sick.
On some days, my character isn’t afflicted with any particular condition, and I’m instead asked to do “social histories.” These scripts aren’t built around any particular diagnosis, but instead are designed to test a medical student’s ability to extract as much pertinent information as possible in the (tragically) short amount of time that most Canadian doctors can allot to any one patient.
For example, I once had to play a mother whose newborn was not eating or gaining weight. The would-be doctors had to ask enough questions to determine that I was a drug addict and a single parent on government assistance, and that I was stressed out for numerous reasons, including the fact that I was living with my extended family since I couldn’t find affordable housing. All of that and more had to be squeezed out of me in less than eight minutes. The same amount of time was assigned to students who had to discover my fake pulmonary embolism, calm me down as I manifested acute grief over the fictional death of one of my parents, and figure out why I had non-existent suicidal thoughts. I have no idea what any of these students thought of my acting skills. But for my own part, I was dumbstruck by the conceit that even trained medical professionals could understand another person’s health needs in eight minutes or less.
I suspect that the students who end up being the best doctors—and perhaps also the ones who will be quickest to burn out—are those who feel most constrained by the time limitations they face. During my acting sessions, the smartest specimens seemed most agitated by the fact the buzzer called time before they’d gotten a chance to ask all their questions.
This past weekend, I had my first opportunity working with pre-med students—nervous undergrads whose scores during these simulations would affect their medical school applications. Unlike actual med-school students, these younger participants were dressed like they were attending a job interview. As they had no medical experience, our simulations proceeded on the idea that they were playing the role of lay administrators and physician representatives in a medical office.
Or, to be more specific, a very woke medical office: According to the script, I was a non-binary LGBT activist demanding that the clinic washrooms be gender neutral. As my instructions read, the “enlightened applicant” would find a solution to my complaint—whether by removing the Men/Women designations or putting tape over the signs. They would also apologize, and work with me to make the office more “inclusive.” Other scripted demands were LGBT Ally signs in the office, posters depicting “people of a gender-fluid appearance,” and staff sensitivity training on LGBT issues.
Internally, I recoiled at my task. As a Canadian who hasn’t even yet managed to find a GP who’ll take me as a regular patient, I was offended by even this fictionalized take on a clinic bending itself into knots for someone prosecuting ideological demands instead of soliciting medical services. These students were effectively being judged on how quickly and slavishly they would prostrate themselves to identity politics. At the same time, though, I owed it to the students to acquit myself professionally. It wasn’t their fault the script had been written by an ideologue. And I was, after all, being paid.

So I aggressively hectored each student about my urgent pronoun needs during their allotted eight-minute simulation. Needless to say, they folded faster than lawn chairs. None of them wanted the equivalent of “ideologically non-compliant” stamped on their med-school applications.
The first young man was so anxious I thought he was going to break down in tears. At one point, he literally blurted out “yes—yes whatever you want.” I felt like I was taking hostages. “Maybe…” One girl nervously gulped, “…we can retrain the staff? Or—or maybe just a whole overhaul?” She was offering to fire the office for me. I could have told her to stand on her head to prove she wasn’t transphobic and I’m pretty sure she would have done it. Not a single student presented any kind of challenge.
Except one—a tall woman with a blue blazer and a pronounced accent (Nigerian, as I later learned). When I told her how urgent it was to cleanse the office of gendered mind-violence, she didn’t panic or blurt out mea culpas like the others. She simply said, “I know you need a bathroom. But some women don’t feel safe around men, too, so maybe we can make a third bathroom for you, okay?”
My script offered me no guidance when faced with someone who offered this kind of common-sense option. Whoever had written it apparently imagined that candidates would either give in, or not give in, but nothing in between—a “false binary,” as some might call it.
I realized that this was the sort of moment that truly tested—nay, defined—a good simulated-patient actor. In a flash, I free-styled, and stitched together the sort of passive aggressive cri de coeur I’d seen a thousand times on Twitter. “Well…I just want to feel included in this space!” I blurted out. “And I don’t care what you have to do to make that happen.”
She nodded and affirmed that she would ask the building management about making a third washroom available, before moving on to my other demands. When her time was up, she slipped out of the room, and I began wearing my internal smile openly. The invigilator, who’d been sitting quietly in the corner till this point, whispered to me, “Not too bad. But what she said was risky, eh?” He scrawled some notes and scored her a nine out of ten, then offered me a kind word: “You had to think on your toes there.”
I took the compliment without offering false modesty in return. After all, he was right. Feigning gonorrhoea or bacterial meningitis is difficult, I suppose. But pulling off the kind of manipulative narcissism that privileges ideological dogma over real community health needs—that’s the mark of a true pro.
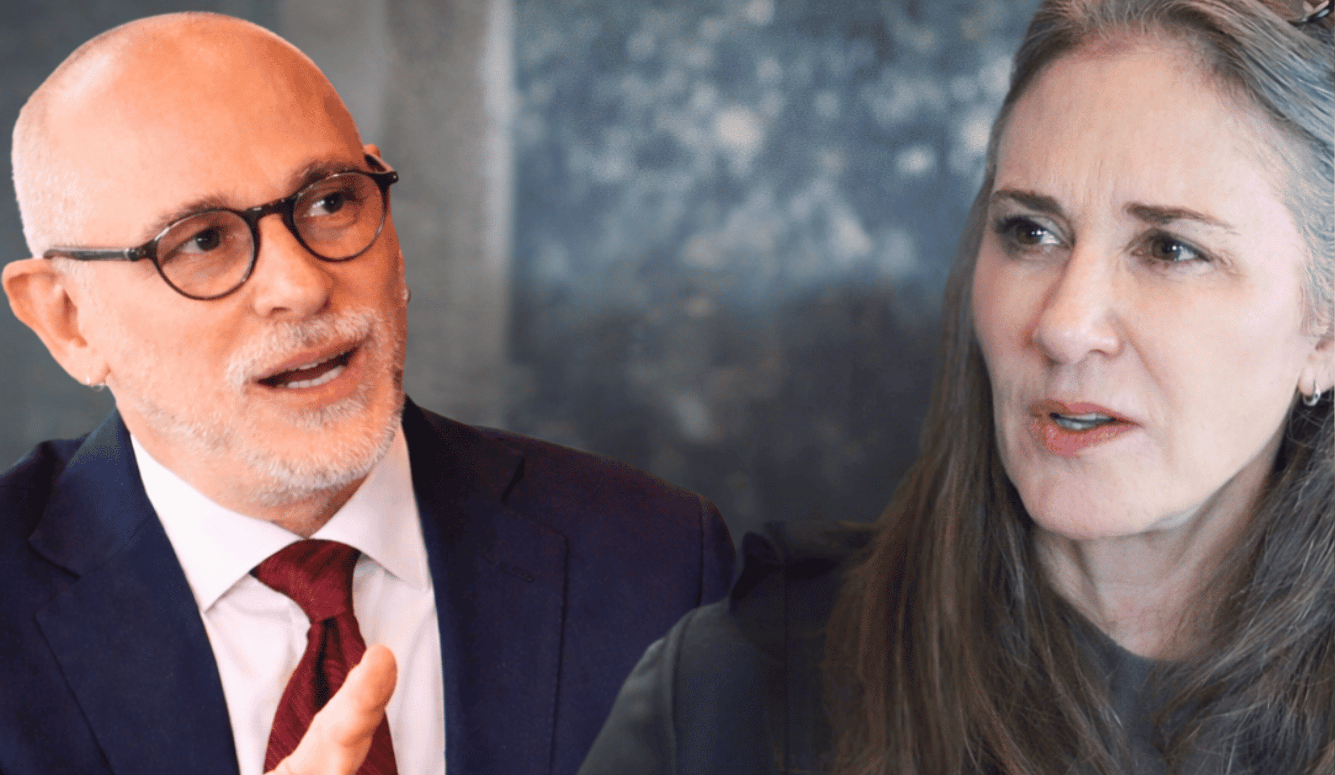
Anna Slatz is a Canadian writer. Follow her on Twitter at @YesThatAnna.