Art and Culture
Risky Business: Public Health and the Culture of Crisis
The goal of public health is ostensibly primary prevention: this means a focus on anticipating, (rather than treating), disease, disorder, and injury.

I. Panic and payment: Funding Primary Prevention
Public health work has become, by nature, reactive. From Ebola to Zika, human health has been sucked into the vortex of the 12-hour news cycle, the details of death by hemorrhagic fever as salacious and gripping as the latest celebrity divorce or gruesome murder. Yet, the real work of public health work is perhaps more sedate and complex than prime-time ratings during an outbreak would suggest.
The goal of public health is ostensibly primary prevention: this means a focus on anticipating, (rather than treating), disease, disorder, and injury. In fact, venerable institutions like the American Public Health Association, the Centers for Disease Control and Prevention, and the World Health Organization at the United Nations exhort public health professionals to not simply eliminate disease or injury, but to actively create the conditions of living that promote a holistic and optimal atmosphere of human well-being, allowing individuals and communities to thrive. All very well-intentioned, if not somewhat oversimplified in the face of public horror as we knock about on the front pages in personal protective equipment reminiscent of 1950s space fiction.
It generally works like this: In order to design the necessary programs, policies, and interventions that effectively abate threats to human health and function, challenges to human health must be identified and responded to, evidence must be rapidly generated and distributed, and the impact of those interventions must be continually evaluated. Add to that the complexities of global politics, the dynamism of sociodemographics, and an often fragmented public health delivery infrastructure, and you have a field that is no longer in the business of vigilance and prevention, but rather in a constant state of crisis response. Quite fun, if you’re into that sort of thing. And considering we’re living longer and healthier lives than at any time before in human history, it’s hardly a failing enterprise.
Obviously, all this firefighting is expensive, and public health work is, largely, publicly funded via federal, state, and local government agencies and cooperative agreements from large international bodies like the United Nations or USAID. From Influenza to HIV, to the infrastructure collapse in Flint, nothing generates funding like a good, old-fashioned public health emergency — and we’re never without the latest, greatest threat. Large, private players like the Bill and Melinda Gates Foundation, Facebook’s Mark Zuckerberg, and The Clinton Foundation are increasingly engaged in the kind of philanthropic work that throws impressive amounts of money into the work of human health. To give you a sense of the reach of this kind of involvement, and the figures involved, The Bill and Melinda Gates Foundation alone cites a foundation trust endowment of $39.6 billion US dollars, with total grant payments into public health work since its inception to 2015 of $36.7 billion, with grantees in all 50 states and the District of Columbia. Internationally, the Gates Foundation alone supports public health-related work in more than 100 countries.
With an intimidating array of areas of public health concern, this private and public money is fundamental to ensuring that everything from staffing, program operations, research, and policy initiatives continue to operate even during times of administrative changeover or politically-motivated economic austerity, when shifts in political dynamics can result in a stranglehold on public funding. Racism, infectious pandemics, gender bias, sexual health and discrimination, chronic diseases like cancer and diabetes, urban and international development, gun violence, suicide, environmental degradation; there are few areas of the human condition that public health work doesn’t touch, and all of them are politically-charged and in need of stable funding. Public health has its own politics, of course, and keeping your job or ensuring the continuity of the service you provide often involves applying for, and winning, competitive grant funding. This means that in order to stay in the public health game you have to really nail one skillset in particular: communicating risk. Those who can convince funders that the sky is falling are those who can, as the kids say, make it rain.
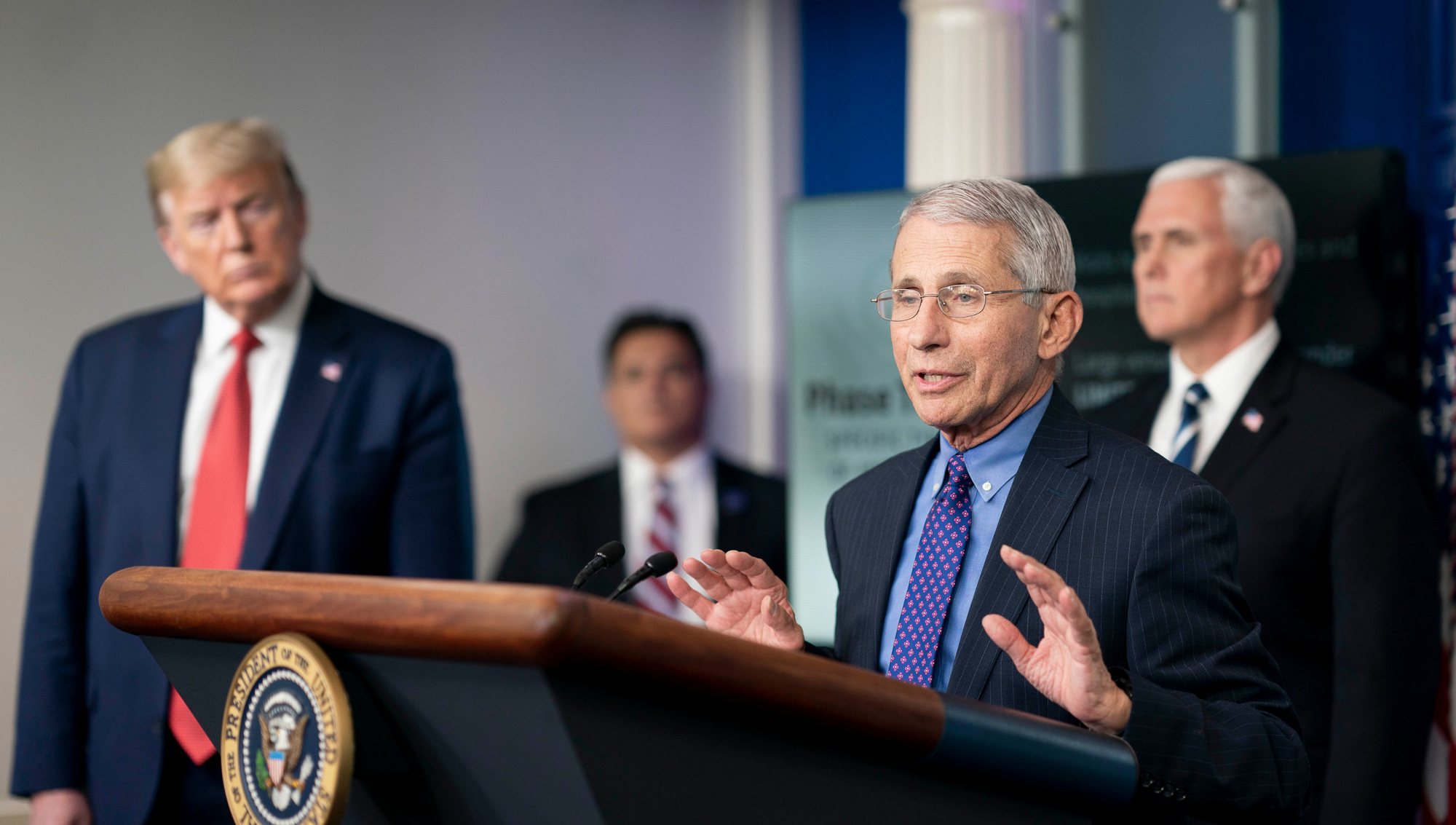
Most money goes to those threats which appear to be most dire and most urgent, those that affect the largest populations, and of course, those that are deemed to be a threat to economic productivity or national security, likely to cause widespread strain on public health infrastructure or panic among the public. Communicating the potential risk of a given public health threat is so fundamental to winning supporting financial awards that entire programs of training are focused on “grantcraft”, and some public health professionals serve the sole purpose in organizations of authoring, acquiring, and managing these awards. Hitting the right panic buttons has become fundamental to institutional and program development in public health.
But the critical importance of risk communication isn’t limited to the interface between researchers, practitioners, and funding bodies. Thousands of experts are specialists in “public engagement” and “risk communication”, examining how to get the right health information to the public and, centrally, persuade them to take a course of action that is recommended by a given public health policy. There are a multiplicity of approaches to accomplishing this, from the public service announcements we’re all familiar with (the Truth campaign against smoking tobacco is a slick, notable, and wildly successful example) to more technocratic approaches that some would argue border on coercion, like “nudging”, wherein the desired health behavior isn’t communicated verbally at all, but rather subtly manipulated via clever environmental design.
Demonstrating proficiency at risk communication to the public is just as central to procuring hotly sought after grant monies as brilliant data demonstrating the genius of your insight is, and while that seems innocuous on its surface, it may be pervading thought in public health in previously unanticipated ways.
II. Crisis or Culture? Anchoring an ethics of risk communication in evidence
It can be said that this endless cycle of problem identification, risk communication, and response sits at the ethical core of this laudable work. We see, we assess, and we respond in the public interest. Simple enough. But what if this crisis-oriented, responsive approach, so apparent and intuitive on its face, is in practice neglecting the fundamental principle of beneficence and prevention? Or violating the ethical standards of public trust, which are nowhere more critical than in the protection of human health? What if, in fact, public health work has become so comfortable in its role in managing and communicating crisis that we’ve begun to manufacture our own?
Let’s take a look at one of the most enduring and wildly successful public health endeavors known to human society: vaccination. Vaccines have prevented a stunning amount of illness and mortality, with many vaccines lowering the death rate since the pre-vaccine era some 99%. And importantly, certain communities and interests in the populations subject to vaccination have always resisted it. And this truly means always, as there’s well-documented historical push-back against vaccines and inoculations from their invention that ranges from honest and well-formed objection to government coercion to flat-out unhinged hysteria about “mind-control”. But in the past 15 years, a less careful observer would be inclined to think that the resistance to large-scale government-backed public health intervention is new, stoked by Jenny McCarthy, an as-of-yet unexplained epidemic of autism, and some very surly soccer moms.

But the general public innocence to the long-standing fight against vaccine isn’t what’s really notable. It’s that there has been a recent flood of consistent messaging coming from the public health establishment that this push-back against vaccines is imminently dangerous, and that the small pockets of vaccine refusers pose a mass threat to public well-being. And while the idea of mass outbreaks of nearly-eradicated disease isn’t outside the realm of possibility given a very specific set of circumstances, the vaccine crisis that has been promoted by the media and leveraged by public health professionals for airtime and funding is largely, in fact, manufactured.
There has been no widespread drop in vaccination rates. While there have been some “pockets” of vaccine refusal and small, well-contained outbreaks and preventable deaths, the situation is far from dire. The CDC is currently reporting that on-schedule infant vaccination rates are close to 99% throughout the United States. Yet, an entire cottage industry has sprung forth to address “vaccine hesitancy” or “vaccine denialism”, with little to no accountability for how much money is being spent to address this issue, or even verification of data that would suggest there’s a problem. So in lieu of well-vetted, data-driven, evidence-based policies with strong evaluative systems for determining the impact of vaccine promotion, we’re really only, if you will, taking shots in the dark.
This is transparently unethical conduct, and a direct result of the culture of crisis with which public health has become comfortable. Never mind that perhaps hundreds of thousands of dollars have been spent with little to no accountability for the effectiveness of vaccine hesitancy research or impact of vaccine promotion programs, and in times of global economic austerity. What’s fundamentally concerning is the research that’s emerging that suggests that un-evidenced approaches to vaccine risk communication can actually make the problem worse, and the willingness of the majority of the public health establishment to proceed anyway, while the getting is good, of course.
III. Calm, clear, and collected: Toward an Evidence-base for risk communication
In 2014, Brenden Nyhan and colleagues published a paper in the prominent journal Pediatrics that found none of a wide variety of communication interventions increased parent’s intent to vaccinate a child. In fact, while the researchers were able to reduce the misperception that vaccines cause autism in the study subjects, exposing parents who had already unfavourable attitudes toward vaccines to risk communication actually decreased their intent to vaccinate. When the researchers showed parents images of sick children, this increased their belief in a vaccine/autism link and in the potential for harmful side effects of vaccines. In short, unconsidered, emotionally-charged rhetoric about vaccination has a decidedly negative effect on getting hesitant parents to vaccinate. And yet, we continue to communicate in this way and to fund these approaches.
While there is currently widespread debate in the public health, social, and biological sciences about the role of and availability of strong, trustworthy evidence and how that evidence should be best used to benefit the public good, the mere existence of good data isn’t enough to inform practice. Rather, a return to the guiding principles and ethical practice of careful primary prevention, even when funding or political restrictions threaten our programs, is needed. Too many of our interventions and programs, public-facing, publicly-funded, and shaping messages on everything from physical fitness to vaccine, are in the “grey literature”, and continue without much oversight from the scientific community or meaningful evaluation of their impact. Surely as we exhort the public to listen to reason and facts we should also be taking reasonable measures to understand the powerful influence funding systems are having on our own practice, and following evidence that suggests our current mode of communication about crisis is ineffective at best and, at worst, unethical.
For now, the case of vaccine risk communication is just that, a case, a curiosity, an illustration of how the constant cycle of crisis management is corrupting public health practice. But with the emergence of novel, potentially devastating pathogens, we must be increasingly mindful that communication about public health threats, and the fight for rapidly diminishing public funding, isn’t a matter of mere words, clever tag lines, and spin. When human lives are at stake, public health communication is indeed a risky business.