Top Stories
Why Have Britain’s Ethnic Minorities Been Hit Harder by COVID-19? It’s Hardly a Mystery
The public-health policies that are put in place in coming years will affect our ability to withstand the next pandemic.

COVID-19 is a disease that can strike anyone. A recent study of 5,700 sequentially hospitalized COVID-19 patients in a New York City health network, for instance, found that patients’ ages ranged from single digits to 90-plus. Roughly 60 percent were male. About 40 percent were white. Nine percent were Asian. And 23 percent were black.
As Coleman Hughes recently noted in Quillette, black people are overrepresented among American COVID-19 fatalities overall. In Chicago, for example, black people account for more than 70 percent of COVID-19 deaths, despite comprising just 30 percent of the local population. But this doesn’t necessarily tell us much about the disease itself, because “black people are more likely than white people to die of many diseases—not just this one. In other cases, the reverse is true. According to CDC mortality data, white people are more likely than black people to die of chronic lower respiratory disease, Alzheimer’s, Parkinson’s, liver disease, and eight different types of cancer.”
In the UK, too, COVID-19 has had a disproportionate effect on communities that get lumped in under the (somewhat dated) term “BAME”—black, Asian, and minority ethnic. The Intensive Care National Audit and Research Centre has reported that 34 percent of a studied group of 6,720 critically ill COVID-19 patients self-identified as black, Asian or minority ethnic. By way of comparison, the comparable figure for a group of 5,782 patients with non-COVID-19 viral pneumonia tracked between 2017 and 2019 was about 12 percent. Moreover, as the Telegraph reports, “despite only accounting for 13% of the population in England and Wales, 44% of all [National Health Service] doctors and 24% of nurses are from a BAME background. Of the 82 front-line health and social care workers in England and Wales [who] have died because of COVID-19, 61% of them were black or from an ethnic minority.”
The release of these numbers prompted an official inquiry. And last week, the Labour Party appointed civil-rights campaigner Doreen Lawrence to head up its own review of the issue. A BBC article entitled “Coronavirus: Why some racial groups are more vulnerable” informs readers that the issue might be rooted in the “physiological burden from the stresses caused by racism and race-related disadvantage, such as the frequent secretion of stress hormones.” London Mayor Sadiq Khan recently wrote an article in the Guardian, demanding that more data be collected. However, he didn’t wait for such data before suggesting that the issue is rooted in “the barriers of discrimination and structural racism that exist in our society.”

I’m a refugee from Afghanistan who came to England as a child in the back of a refrigerated truck. So I know a little bit about these issues. I also know that the above-described statistical disparities may well be related to factors that have nothing to do with racism. Firstly, as everyone in the country knows, BAME communities are disproportionately urban. Specifically, they tend to live in Britain’s larger cities, such as London, Birmingham, and Manchester—often within populous urban wards. Contagion rates are high in these areas, in part because it’s easier for an epidemic to spread in a big city than in the country’s sparsely populated (and disproportionately white) countryside.
Secondly, BAME groups in the UK tend to have more aggravating health conditions, known as comorbidities. Given the epidemiological data, this is of enormous importance. In the aforementioned study of 5,700 COVID-19 patients in New York City, for instance, the leading comorbidities were found to be hypertension (57 percent of all patients), obesity (42 percent), and diabetes (34 percent). Overall, a stunning 94 percent of patients in the study had at least one comorbidity. And 88 percent had more than one.
According to 2006 data, South Asians in the UK are up to six times more likely to develop type-2 diabetes as compared to white people, and black people were up to five times more likely. Similarly, as the BMJ has reported, people of South Asian and Black ethnicity “are known to have worse cardiovascular outcomes than those from the white British group”—in large part because of the “significant” effect of differences in average hypertension levels.
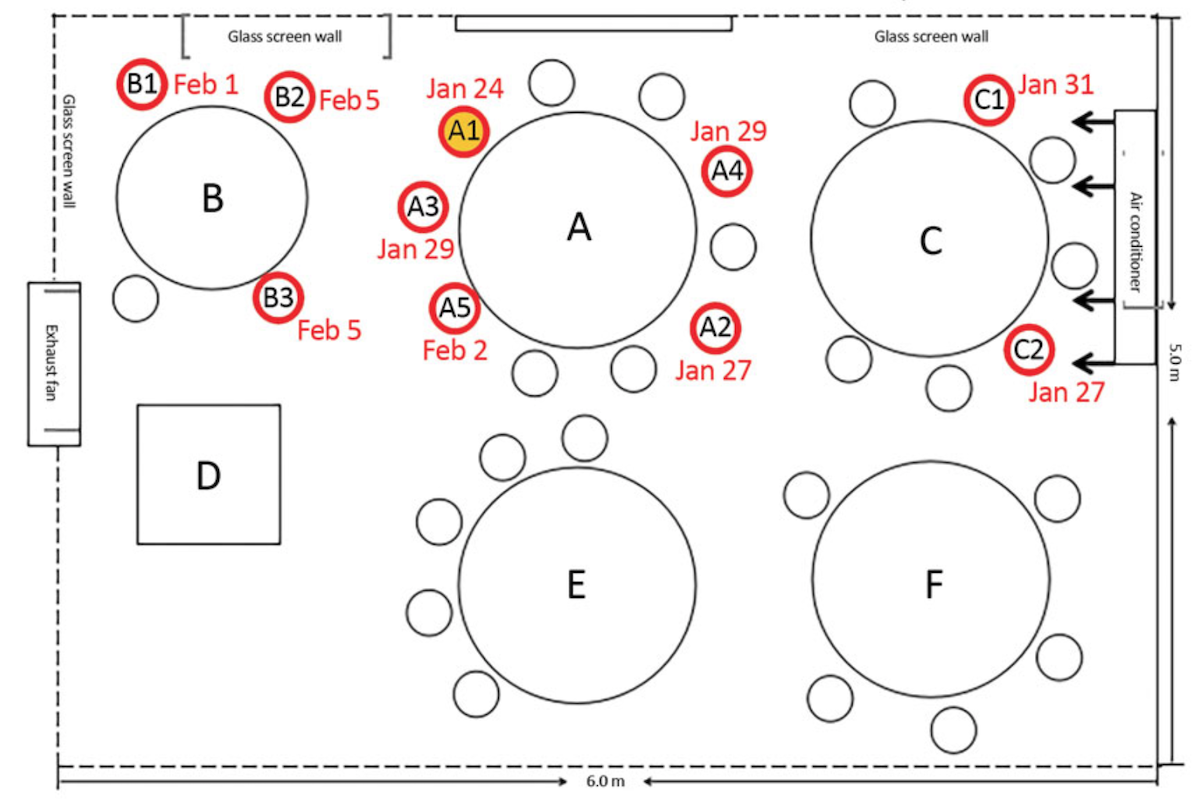
Thirdly, immigrant households are far more likely to contain more than two generations living under one roof. (The authors of a 2017 report found that 70 percent of surveyed white households in the UK containing people aged 70-plus didn’t contain younger individuals. The comparable figure for black households was about 50 percent. For South Asians, it was 20 percent.) In such circumstances, social isolation is more difficult, and grandparents are put at risk of catching infectious diseases from (possibly asymptomatic) younger relatives. From the beginning of this pandemic, intra-household contagion has been a leading form of COVID-19 transmission. The bigger the household, the more people get infected in each cluster.
Fourthly, the problem of getting public-health information to citizens is compounded in the case of those immigrants who have limited English abilities. There is much less official information in Somali, Hindi, Farsi, or Pashto, for instance. There is lots of “fake news” circulating on WhatsApp groups, which is especially problematic in the case of those who don’t understand information coming from official channels in English. Much of this fake-news information flow flies under the radar of public officials.
Finally, as noted above, BAME workers make up a disproportionate share of National Health Service medical staff. A fifth of nurses and midwives, and a third of doctors, are from BME backgrounds. In many cases, these actually represent employment success stories. But as one would expect, these cohorts also tend to be younger, and so are disproportionately employed in entry-level roles and front-line care, as opposed to working in specialized clinics or managerial positions.
An objective assessment of such issues is welcome. But the government’s fact-finding project should take into account the underlying factors, as opposed to simply echoing some of the unhelpful generalizations that now have become common currency in the media.
The public-health policies that are put in place in coming years will affect our ability to withstand the next pandemic. And we should be mindful of the manner by which they impact different communities in different ways. Such a discussion would not only help save lives, but also help spark a larger discussion about why such differences continue to exist, and, more generally, what factors have prevented BAME communities from sharing in the benefits that come with social integration.