The Philadelphia Experiments
How an enterprising doctor, an elite university, and negligent public officials turned a city prison system into the largest human research factory in America.
I.
When La Salle University student Priscilla Morris first came across the 1971 portrait of Dr. Albert M. Kligman in Philadelphia’s Woodmere Museum, she says she found it “eerie. I really thought the portrait quite ominous.” For Morris, a criminal justice major doing a deep dive into Kligman’s controversial career, the portrait confirmed her opinion of the renowned University of Pennsylvania researcher as “menacing.” The woodblock print by Kligman’s second wife, Mitzi Melnicoff, divides his face into red and yellow, marked by bold, slashing black lines. The result is dramatic. Some consider it unsettling and off-putting. Melnicoff said she wanted to emphasize her husband’s “powerful force of character,” but she may have gone too far. Morris is probably not alone in finding something sinister about the picture—a quality familiar to those, both free and behind bars, who had the dubious pleasure of meeting its infamous subject or being used as his research material.
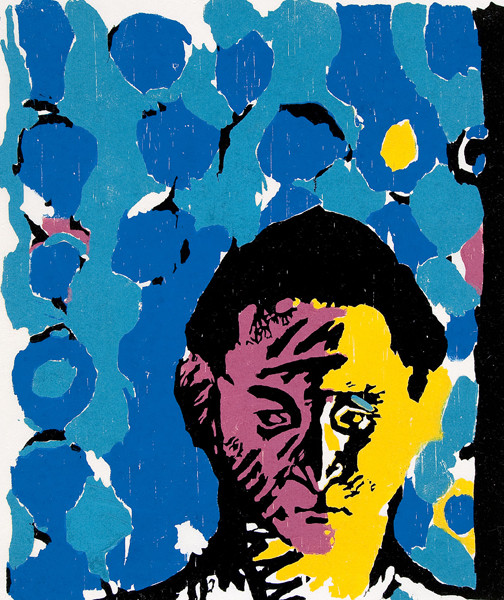
Melnicoff’s portrait was painted at a time when her husband was riding high. A one-time enfant terrible of the medical/academic arena, he was now comfortably ensconced at a prestigious Ivy League University, the author of dozens of medical journal articles and several books, and the go-to scientist for numerous pharmaceutical companies conducting Phase I drug trials. By the early 1970s, he was well on his way to being recognized as one of the world’s most influential dermatologists.
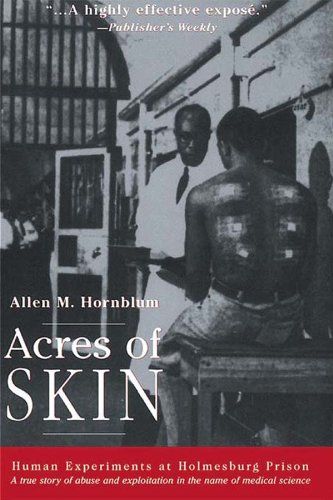
Dr. Kligman would die in 2010 at the age of 93. His New York Times obituary described his many accomplishments and the critical role he played in bringing a “scientific base to dermatology.” It mentioned his “innovative” and “very charismatic” personality, his coinage of new terms such as “photoaging” and “cosmeceuticals,” and his wildly profitable commercial products, Retin-A and Renova. However, the Times also mentioned my book, Acres of Skin, which illuminated Kligman’s darker side—his use of vulnerable populations for medical research and the many “ethical questions that dogged his career.” In fact, the last 10 years of his life would be, in some respects, a bulwark action in defense of his scientific contributions as he fended off attacks that cast him as a modern day Mengele, who used institutionalized black men as grist for his research mill and personal enrichment.
Kligman’s reputation and the research empire he created had already taken a number of hits when, on October 6th, 2022, Philadelphia became the first city in the nation to apologize “to those who were subjected to the inhumane and horrific abuse” in the county’s correctional system. Recognizing “the historical impact and trauma of this practice of medical racism” and the “deep distrust experiments like this have created in our communities of color,” Mayor Jim Kenney “formally and officially” extended “a sincere apology” for this “deplorable chapter” in the city’s history. That apology, which recalled President Bill Clinton’s 1997 apology to the survivors of the infamous Tuskegee Syphilis Study, received widespread media coverage, including in publications in the United Kingdom, France, and China.
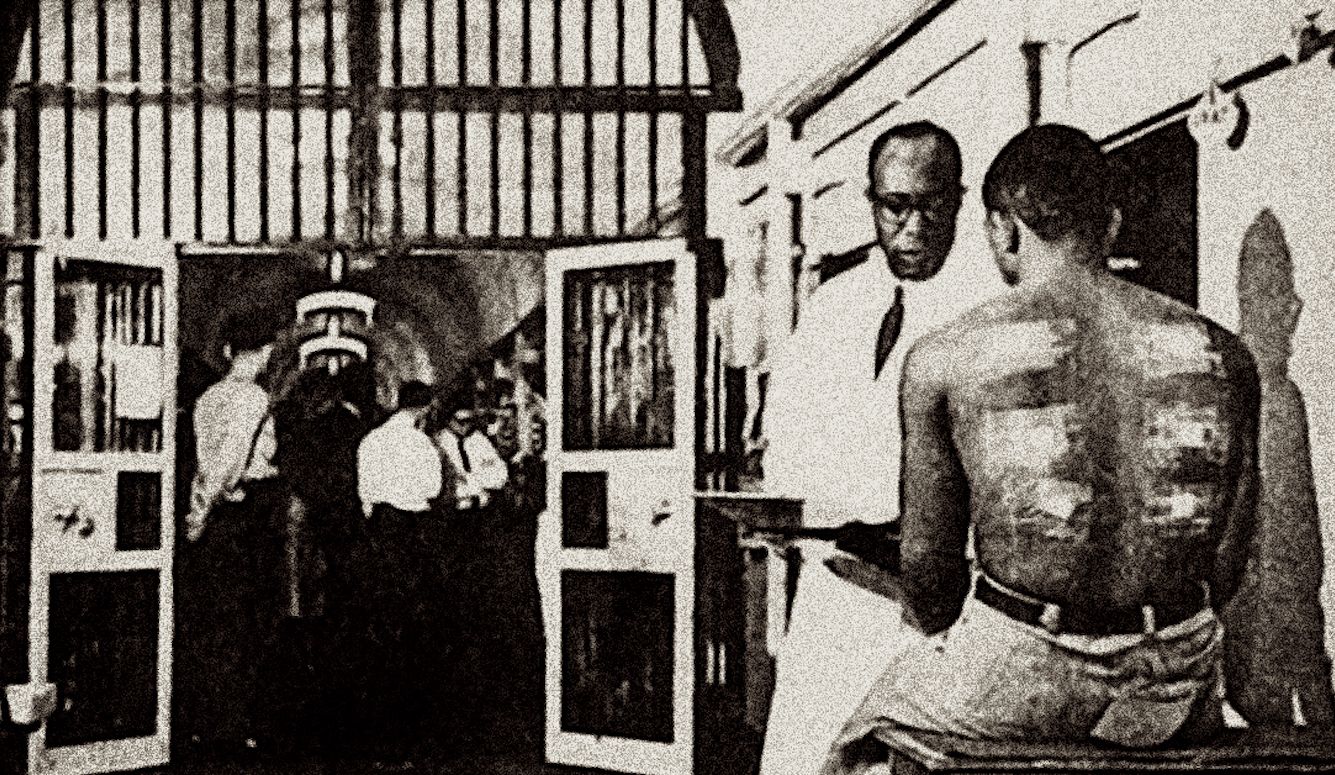
But back in 1971, when I obtained a job working in the Philadelphia prison system as the director of its adult literacy program, Kligman’s human experimentation factory was humming along smoothly. Holmesburg prison was as wildly raucous, putrid, and threatening as I had anticipated. What I hadn’t expected to see were scores of inmates adorned in medical dressing. Prisoners’ arms, chests, and backs were strapped and wrapped in adhesive tape, bandages, and gauze pads, and they paraded through the institution’s corridors and cellblocks as if they’d just returned from a battlefield. To a 23-year-old novice just out of graduate school, the sight was unnerving.
“What’s with all the injured prisoners in gauze pads and medical tape? Is the place really that dangerous?” I asked John Reeves, a black correctional officer on A Block. “Oh, that’s nothing,” he replied with a chuckle. “That’s just the perfume tests for the University of Pennsylvania.” Reeves explained that Kligman’s tests had been a common feature of Philly’s prisons for 20 years. “You and I wouldn’t get involved with this testing bullshit,” he barked impatiently as he began to weary of my questions, “but these inmates are crazy. And they’re desperate for money. These experiments are the only way to make any money in the jail.”
What I was starting to understand—but would not fully comprehend until two decades later—is that the Philadelphia Prison System had been hijacked by Kligman, who saw the hundreds of inmates languishing on stifling cellblocks as ideal subjects for medical research. From his first visit to the jail in 1951, he realized he had found a large disposable cohort for experimentation. Best of all, this “anthropoid colony … under perfect control conditions” was sequestered behind a 35-foot fieldstone wall.
So, he ingratiated himself with the prison overseers and set about transforming a critical portion of the city’s criminal justice system into an adjunct—if not a wholly owned subsidiary—of Penn’s Medical School. Looking back years later, Kligman nostalgically remarked, “I began to go to the prison regularly, although I had no authorization. It was years before the authorities knew that I was conducting various studies on prisoner volunteers. Things were simpler then. Informed consent was unheard of. No one asked me what I was doing. It was a wonderful time.”
The lack of city oversight combined with a researcher’s unrestrained curiosity and keen commercial instincts provided the recipe for an ethical calamity. Initially, Kligman performed rudimentary academic clinical trials consistent with his job as a medical school professor. Consequently, Holmesburg gradually became a valuable training ground for Penn med students hoping to embark on careers in dermatology. Before long, however, Kligman’s prison testing program was involved in an array of research projects that ran the gamut from the mundane to the bizarre. And as his reputation grew, he attracted the attention of commercial entities looking for cheap and available test subjects who could assist in the development of new products.
Protocols testing soap, toothpaste, hair dye, deodorant, detergent, shampoo, and other assorted oils, lotions, and creams, began to overtake Kligman’s academic agenda. Money, he soon discovered, could be made from what he called the Philly prison system’s unlimited “acres of skin.” The entire enterprise, as Dr. A. Bernard Ackerman would argue years later, became dedicated to commerce. A one-time protege of Kligman’s, Ackerman would go on to become one of the world’s leading dermatopathologists. His mentor, he later declared, was a fraud and he labeled the Holmesburg Prison research project “little more than a commercial operation in which Dr. Kligman, the University of Pennsylvania, and others, reaped huge financial dividends.”
II.
Some of Kligman’s experimental studies were unusual enough to attract media interest. In the mid-1950s, Life magazine covered Kligman’s pursuit of an elixir he hoped would become the “the first practical poison ivy immunizer.” The three-page story—probably the first for a dermatologist in a national magazine—was titled, “The Poison Ivy Picker of Pennypack Park,” and featured photographs of Kligman on his knees collecting the dangerous plant in a nearby park. Other stills captured inmates lining up to receive his experimental vaccine, having poison ivy plant leaves rubbed on their arms and legs, and the ugly rashes that resulted.
Less advertised were other Kligman experiments that put inmates at even greater risk. In Acres of Skin, I recorded that:
A 1958 study inoculated scores of prisoners with such ectodermotropic viruses as wart virus, vaccinia, herpes simplex, and herpes zoster. The subjects of these experiments were “healthy colored male volunteers, 20 to 45 years of age” who volunteered to be “inoculated” several times. In the wart virus section of the study, “47 inoculations were performed in 7 volunteers in different skin areas (forearm, palm, … back, face, scalp, … and penis). All of the recipients developed at least one lesion, some of them two lesions at different localizations.” [Quotations from Herbert Goldschmidt and Albert M.Kligman’s paper, ‘Experimental Inoculation of Humans with Ectodermotropic Viruses,’ Journal of Investigative Dermatology (September 1958)]
Why would men agree to have poison ivy rubbed on their arms and thighs, wart virus injected in their face and penis, and endure other uncomfortable indignities? The answer is simple—they were incarcerated and there was money to be made “guinea-pigging” in Kligman’s experiments. With money on the books, an inmate could acquire potato chips, candy, and toiletries from the prison commissary, send a few dollars to a wife or girlfriend, obtain an attorney, or with enough tests, make bail. Jobs in jail were rare and the pay was pitiful. Pushing a broom on a cellblock earned an inmate 25 to 50 cents a day—what was known as “chump change.” But the medical experiments paid a dollar or two a day; princely wages by prison standards. Some, like the army experiments that started in the early 1960s, paid even better.
Though they were rarely told the truth about what was being administered, inmates knew there were risks. Poorly educated, prone to risky behavior, and in need of cash, prisoners nonetheless gambled on the honesty and benevolence of the Ivy League doctors in white lab coats with MD and PhD after their names. The tests were harmless, they were assured, and there was no need to worry. “These Penn doctors are the best around,” one seasoned con with six gauze patches on his back told me at the time. “And besides, I’ve put enough crap in my veins and body these doctors ain’t gonna hurt me.”
The program’s appeal was greatest among the poor and less educated. Some inmates in need of cash allowed themselves to become party to Kligman’s penchant for dermatological curiosities. William Harper, for example, was paid $50 to let Kligman transplant a piece of his lip to his upper arm, and a piece of skin from his upper arm to his lip. “Hop” as he was known in the jail, told me he was never informed of the reason for this strange surgical exercise, but appreciated having money on the books. Those with resources and a higher level of academic attainment shunned such overtures. “You gotta be a fool to get involved with that shit,” was a common refrain from those who refused to take part in Kligman’s program. Then there were some like Chick Goodroe, a prolific burglar with money on the books, who occasionally volunteered just to get off his cellblock. “I had money,” said Goodroe, “but looked for a test that seemed safe and allowed me to get out of my cell and stretch my legs.”
Interestingly, the racially separatist Nation of Islam preached non-compliance and forbade its members from participating in the medical research program. “Those Penn doctors are using the black man as human guinea pigs,” said Clarence Fowler, a convicted murderer and the leader of the Black Muslims in the Philadelphia Detention Center. “It’s just like the Jews in Nazi Germany,” he said. “Nothing but the black man’s destruction will come of it.” Steeped in racial hatred and distrust of white doctors and their experiments, the Muslims at least proved to be prescient on the subject of prison research.
The bulk of the prison population, however, was receptive. And there was no shortage of opportunity; clinical trials were beginning to rival criminal justice as the county prison system’s raison d’etre. By the early 1960s, the Penn dermatologist had solidified his position as the country’s most prolific researcher. His prominence was soon noticed by government officials. When I asked Dr. Alan Lisook, the former chief of clinical investigations for the Food and Drug Administration, about the prison program, he replied, “Kligman may have done more testing than any other doctor in America. If he wasn’t number one, he was up there.”
Some of the nation’s most widely known and respected corporations sought the Penn physician’s assistance. Business relationships flourished, and were usually long-maintained, though some proved unsatisfying. In 1964, for example, Dow Chemical found themselves in a jam. A factory at their Midland plant in Michigan that produced a popular herbicide was forced to shut down when dozens of employees came down with chloracne—skin outbreaks caused by dioxin exposure. Fearing that their health was threatened, workers walked out. The union said their members would refuse to return until the problem was fixed. Increasingly concerned, company officials leaned on in-house scientists to identify and rectify the problem so that production could resume.
Dow doctors and chemists suspected that the contaminant 2,3,7,8-tetrachloro-p-dibenzodioxin (TCDD) was the probable cause of the chloracne. They knew the substance was dangerous, as it had already been linked to cancer and birth defects. Tests on rabbits’ ears appeared to confirm their suspicions. But company managers wanted results from tests on humans. Where did one go in the 1960s to have such clinical trials conducted? They went to Philadelphia. Dow contacted Kligman, who was known to have tested various chemicals on prison volunteers in Pennsylvania, and in December 1964, the physician traveled to Michigan to listen to a presentation by Dow officials about their chloracne dilemma.
Kligman accepted the challenge in short order. For a $10,000 fee, he agreed to find the threshold dose that impacted humans and assured the company that he would assume full responsibility for any liabilities. He then created a waiver for the prisoners to sign which stated:
I, the undersigned, also hereby give my permission to the hospital, laboratories, or others to perform medical and other tests on me: the hospital, laboratories, etc. or the prison are not to be held responsible in any way for any complications or untoward results that may arise.
Protected at both ends now—especially since inmates were not told what was being applied to their skin—Kligman began his experiments. This was probably the only time that a dioxin was scientifically administered to American citizens.
Dow sent Kligman a very conservative protocol to follow, and a small amount of TCDD with the clear warning; “Danger! This material is extremely toxic.” Inmates were recruited for the study and had the chemical applied to their foreheads and backs, but the results were unsatisfactory. Disappointed, Kligman wrote to Verald Keith Rowe, the Dow executive who contracted him to do the study, to inform him of “the astonishingly negative results … the test agent gave no evidence of being acnegenic and was not harmful to the subjects.”
While decision-makers at Dow pondered their next steps, Kligman took it upon himself to press on. Unilaterally, he decided to alter the protocol, increase the dosage 468 times, and initiate another round of tests. Unsurprisingly, the test subjects came down with “acne form lesions … and inflammatory pustules and papules.” Kligman was delighted, but Rowe was shocked when he learned what had been done. “His protocol was quite amazing,” said Rowe, when I tracked him down in retirement. Kligman’s actions caused us to “sever the relationship. He didn’t give us any notice.” Rowe admitted Dow scientists were “quite startled” by Kligman’s recklessness, which had basically ensured that test subjects would have their health compromised.
Rowe’s replies to my questions were frank and succinct. Why didn’t he contract research physicians in Michigan as opposed to hiring someone in Pennsylvania? “I didn’t know about any prison testing in Michigan, and Kligman was a known quantity. He was somebody with a strong academic reputation.” Did he have any concerns about the disproportionate number of African Americans in Kligman’s original protocol? And why did Dow accept minimal evidence of informed consent? “I didn’t have too much of a problem with Kligman’s operation in that regard. That was his area of concern. The protocol was my business. I knew what I wrote and what I wanted.”
Kligman was more troubled by the loss of a corporate relationship and the money it brought in than he was by any threat to inmate health. He was not oblivious, however, to the dilemma clinical trial operators faced. “We had an ethical problem,” Kligman admitted later. “How much right do you have to cause risk to a prisoner in medical tests from which he has no direct benefit? All the prisoner taking part in the test has is money. We pay him to lend us his body for some time. But we pre-determine whether a test is dangerous, and the prisoner has to depend on our judgment.”
But for the Penn professor, this moral conundrum seems to have been quickly and easily hurdled. “The prison,” said Kligman, “is the right place for such a test.” He’d even go on to offer a “humanitarian” justification for his conduct, arguing that inmates derived benefits from participating in his clinical trials and associating with his complement of dedicated doctors on the cutting edge of great medical advances. But he wasn’t unmindful of his own power and influence in the well-oiled human testing machine he had created. As he told one newspaper reporter in the mid-’60s when his program was experiencing unprecedented growth, “I feel almost like a scoundrel—like Machiavelli—because of what I can do to them.”
Fifteen years later, during the growing controversy surrounding the use of Agent Orange in Vietnam, the secret Dow-Holmesburg dioxin studies were finally revealed. Initially, there were newspaper headlines and expressions of concern from various quarters, but interest was fleeting; the victims of that benighted scientific exercise were, after all, prison inmates. The government took note of the declining news coverage and adopted a minimalist approach to investigating the matter. Naturally, Kligman claimed that his files and documentation had been destroyed in a fire. The dozens of Philadelphians who had been dosed with a dangerous carcinogenic chemical would remain ignorant of how they had been used. No one ever learned who they were, and no one cared.
III.
The Dow Chemical fiasco and the deception behind it was just one of many disasters Kligman foisted on the prison system, the thousands of people interned there over the years, the city administration that allowed him to operate, and an elite university that seems to have accepted a Faustian bargain with their enterprising but ethically challenged colleague.
During the 1960s, Kligman’s reputation as a researcher-for-hire, and Holmesburg’s open-door policy towards clinical trials grew the business exponentially. A new chapter was being written in the convict labor saga. Prisoners were no longer rented out to plantation owners and mining companies for backbreaking chain-gang labor clearing canals or digging mine shafts and irrigation ditches as they did in the deep South at the turn of the century. Now, they were sitting on prison cellblocks and in hospital metabolic wards swallowing pills and being injected with new investigational drugs; raw material for pharmaceutical companies in need of Phase I drug trials.
An academic star at the nation’s leading school of dermatology, and landlord of the country’s largest and busiest human experimentation bazaar, Kligman was like no other medical professor in post-war America. Former students talk of his “brilliance,” his “genius,” and describe him as an “absolutely unique individual” who was “just exploding with ideas.” They were also struck by his flair and exaggerated self-confidence. “He told students that rules don’t apply to genius,” said Dr. Paul Gross, “they just get in the way of creative minds.” Gross observed Kligman first as a student and then a colleague and was impressed by his mentor’s showmanship and chutzpah. “He thought he could do and say anything and get away with it because he was superior to the average fellow and deserved greater freedom. As a student I believed everything he said.”
“I was a big Kligman fan,” Dr. Ackerman told me. “He was famous and had a lot of style and pizzazz.” Ackerman recalls that when he first met the famous dermatologist at a medical conference in Miami in 1965, Kligman was outgoing, personable, and delightfully entertaining. “He told me and other students looking for a high quality medical residency at a top school, ‘Come to Penn, we have acres of skin.’” The two men became close. “Kligman,” Ackerman told me, “was the most interesting man in dermatology. Nobody was as dashing and as exciting. He was a dominant figure—he was intriguing and was alive intellectually. All of the residents modeled themselves after Kligman.”
An accomplished gymnast during his time as an undergrad at Penn State, Kligman was also an enthusiast of airplanes, motorcycles, tennis, horseback riding, and a riveting raconteur. He would go on to earn a PhD in botany at the University of Pennsylvania, before deciding a life in the weeds studying plant fungi was not the exciting and financially rewarding career he wanted. He went back to Penn’s medical school for his MD and began churning out journal articles on fungus in humans.

Titles such as “Improved Technique for Diagnosing Ringworm Infections and Moniliasis,” and “The Hotchkiss-McManus Stain for the Histopathologic Diagnosis of Fungus Disease” weren’t about to capture the public’s imagination, but they did catch the eye of a Holmesburg medical staffer struggling to contain a nasty epidemic of athlete’s foot at the prison. He contacted the young fungus expert for guidance and the die was cast. Far more enterprising and visionary than the average post-war med-school prof, Kligman immediately perceived the prison’s full academic and commercial potential. He later recalled that when he walked through the institution’s 15-foot-high front doors and saw hundreds of aimless, captive men, “It was like a farmer seeing a fertile field for the first time.”
Like many others impressed with Kligman’s energy, creativity, bold opinions, and self-assurance, Ackerman was swept off his feet by the man’s unique aura. His freewheeling use of a city prison system as a clinical training ground only seemed to underscore his creativity and elite status. But one day, while giving his brother, a Penn orthodontist, a tour of the facility and the experiments underway, he experienced an epiphany. His brother pulled him aside at the end of the visit and soberly inquired, “Have you ever heard of the Nuremberg Code?” Ackerman was taken aback and immediately began re-examining what he was doing, where it was being done, and who it was being done to. And for whose benefit? The answer to those questions and others proved unsettling and eventually soul-searing. When the academic year was over, Ackerman withdrew his residency at Penn and transferred to Harvard.
Few people, if any, challenged Kligman to his face. He was rightly feared for his ability to destroy friend and foe alike with brutal ad hominem attacks. His verbal skills, intensity, and professional stature made him practically unassailable. But students took note of his bluster and callousness nonetheless. Dr. Margaret Gray Wood, a former Kligman student and, many years later, chairwoman of Penn’s Dermatology Department, told me stories of his periodic insensitivity to her classmates and test subjects. Wood recounted Kligman’s classroom comments when discussing his use of physically and intellectually impaired children at the Vineland and Woodbine centers in South Jersey for his research endeavors. Kligman, Wood recalled, often described how he “encouraged the development of ringworm by rubbing it in the abraded scalp of retarded children.” He would delight in informing medical students and residents-in-training that, “These kids want attention so bad, if you hit them over the head with a hammer they would love you for it.” Students flinched and fidgeted in discomfort, Wood said, but most just chuckled nervously—it was just another of their cocky professor’s off-color jokes.
Kligman’s move from using four-, five-, and six-year-old children at the New Jersey State Colony for the Feebleminded for various experiments in the late 1940s to using inmates at Holmesburg Prison in north-east Philadelphia in the early ’50s required no great leap. If marginalized children were legitimate grist for the experimental mill, imprisoned adults would certainly be acceptable. In fact, the geographical shift saved Kligman considerable travel time and allowed him to expand his ever-burgeoning field of research interests.
IV.
Back in the early 1970s, I was unaware of any of this. I had no idea of Kligman’s larger-than-life persona, his many books and journal articles, or his unrivaled status as a dermatological comet in the medical firmament. Nor was I aware of his brazen dioxin experiments, the radioactive isotope injections administered to unwitting prisoners, his deception of the Atomic Energy Commission, or his pivotal role in helping the US Army’s Chemical Corps perform dangerous mind control, skin hardening, and chemical warfare experiments on hundreds of prisoners for over a decade.
These and the countless other Phase I drug trials were a roiling blur to us. Those of us who worked in the jail saw the test subjects adorned in tape and gauze pads, the white-robed medical personnel, the occasional visits by military officials, and the inmates in lab coats handing out medication as if they were trained hospital staff. But we had no idea what was actually going on. As in most government-run paramilitary operations, everyone had bought into the program; if it was okay with the prison wardens and the politicians downtown, it was okay with us. Even inquiring about the research was considered bad form, if not taboo.
But I knew there was a story there and fully anticipated that one day a journalist or historian or medical ethicist would delve into the University of Pennsylvania’s prison research program and publish a book or report that told all. Years passed, then decades, and still nothing emerged; it had become increasingly obvious that if I didn’t tackle the subject myself it would never be addressed. I was still running into many of the men I first met in the jail 20 years earlier. As chief of staff of the Philadelphia Sheriff’s Office in the early 1990s, I’d occasionally spot inmates in our City Hall cell room who I knew many years earlier as prisoners. Some of them had been test subjects. I began pulling them aside, asking what they recalled. They were willing to talk, recounted stories, and some even showed me the blotches, scars, and strange markings they still carried from the tests in which they had participated.
I began tracking down current and former prisoners in local and state penal institutions as well as those on the street. Their accounts of Kligman’s program were illuminating and occasionally shocking. I then pursued the physicians and their research assistants to get their side of the story. The replies were revealing. “I won’t talk unless I can have a lawyer present,” “I’ve been dreading this call for years,” and “Please don’t name me in anything you write” were just a few of the comments I heard. There were also angry threats, and in one case, the sound of a telephone receiver being slammed down. A troubling pattern emerged: former inmate test subjects were willing to talk, but knew nothing of the operation in which they had been involved. Doctors who knew the score, on the other hand, were unwilling to talk. That mystery only whetted my appetite.
I conducted scores of interviews and committed myself to a serious exploration of human experimentation in America. That history, I discovered, was like a pockmarked battlefield; a few periodic triumphs littered with nameless corpses. The great men of science—Walter Reed, Theobald Smith, Hideyo Noguchi, and Joseph Goldberger—were faintly familiar, as was their heroic role in conquering diseases like yellow fever and pellagra. But I now also learned of the hundreds, if not thousands, of people who became the cannon-fodder for their celebrated campaigns. The unattractive calculus of medical research back then was becoming increasingly apparent. As Walter Reed told one of his chroniclers, “To make any kind of experiment to prove mosquitos carry yellow fever, you must have experimental animals, and that meant nothing more nor less than human animals.”
Federal, state, and local prisons were often the destinations of choice for doctors in search of some magical elixir, life-saving potion, or simply a means of advancing their academic careers. Ingratiating oneself with the pharmaceutical industry came later. As Dr. Lisook, who kept track of such things for the FDA told me, “Prisoners were used because they were cheap and nobody gave a damn what happened to them.”
Penal institutions with high-profile reputations such San Quentin, Leavenworth, Sing Sing, and dozens of lesser known institutions all hosted medical research projects. Virginia State Penitentiary was conducting flash burn studies; Terre Haute and Seagoville Federal Facilities were hosting studies on sexually transmitted diseases; Stateville in Illinois gave inmates malaria; Ohio State Pen conducted cancer studies. At least half the states in America had at least one prison hosting clinical trials of one kind or another, but Pennsylvania held the record. And at least a dozen penal facilities were exploiting prisoners as experimental test subjects, but Philadelphia was the crown jewel of the non-therapeutic, for-profit business model. Anything anybody wanted done could be accomplished there. Kligman, the University of Pennsylvania, and elected city leaders turned the county correctional system into the Macy’s of human experimentation. And though it went on for a quarter-century, no one—certainly no one of prominence—seemed to find the practice troubling.
The willingness of so many people to buy into something so morally reprehensible fascinated me. I looked into the notorious Tuskegee experiment conducted in Alabama between 1932 and 1972, which studied the effects of untreated syphilis in 400 black males, 100 of whom died. How was it possible, I wondered, that no one in the medical community raised a concern about hundreds of sick men going untreated for 40 years? Unschooled, impoverished, and afflicted with “bad blood,” black sharecroppers in Alabama were closely monitored by the United States Public Health Service (USPHS) on an annual basis, but were prevented from receiving state-of-the-art medical treatment that would have alleviated their suffering. Apparently, no one in Alabama or the USPHS thought to object to such an obviously racist and unethical project. Nor did the countless number of physicians who read the dozen or so medical journal articles over the years informing readers of the study’s findings. The Holmesburg experiments—Tuskegee’s flip side, in which healthy men were made ill—produced a similar silence.
In search of an explanation for this apparent indifference, I sought out some of the nation’s top scientific investigators. Among them were controversial scientific figures such as Chester Southam, Hilary Koprowski, and James Ketchum. Contrary to my expectations, Dr. Southam, who was infamous for his cancer injection studies of inmates at Ohio State Penitentiary and elderly patients at the Jewish Chronic Disease Hospital in Brooklyn, turned out to be kindly, gentle, and welcoming. He was in his mid-70s when we met, and maintained that his Sloan-Kettering research projects weren’t as unethical and dangerous as his critics made them out to be. When I asked him about the Nuremberg Code, he shrugged. “I was unaware of the Nuremberg Code and its code of conduct,” he replied. “All I know is that the prison research was valuable, and the publicity regarding the prison experiments was favorable.”
Dr. James Ketchum was a psychiatrist for the US Army who conducted a series of secret psychopharmacological and mind-control experiments on soldiers and prison inmates. Ketchum held degrees from Columbia, Cornell, and Letterman and Walter Reed Army Hospitals, but he offered the same defense. “There was very little, if any, emphasis on the Nuremberg Code in my academic and clinical training,” he recalled. Even Bernie Ackerman, who would become a staunch supporter of increased ethics training and an outspoken critic of Kligman and the Holmesburg program, said the same. Ethics generally, and the Nuremberg Code in particular, he said, had no role in his medical education. Yet it will be clear to anyone who reads the first principle of the Nuremberg Code crafted by American jurists at the Nazi War Crimes trials in 1947, that “the voluntary consent of the human subject is absolutely essential.” The test subject must also have “free power of choice, without the intervention of any element of force, fraud, duress, overreaching, or ulterior form of constraint or coercion.”
Regrettably, the American post-war medical establishment chose to devalue the newly drafted ethical code just as it devalued the many powerless, institutionalized people used as research material. The Nuremberg Code, they argued, was for Nazis, not American doctors and researchers. “A utilitarian ethic continued to govern experimentation,” argued medical historian David Rothman, “partly because the benefits were so much greater than the costs.” The confluence of self-interest, consequentialist thinking, and the needs of science and medicine militated against the American medical community’s embrace of the Nuremberg Code. Granted, the lack of ethical guardrails helped propel a “golden age of science,” but at what cost to those used as research subjects?
V.
After five years spent conducting interviews and pursuing incriminating documents—especially those garnered through extensive use of the Freedom of Information Act—Acres of Skin was published in 1998. The book received extensive media coverage, and it finally allowed the former Holmesburg test subjects to understand how they had been exploited and what experimental potions, concoctions, and drugs they had been given. Their shock and moral outrage was understandable. They had placed their trust in doctors and a prestigious medical school, and were reassured that no harm would come to them. There was no mention of Phase I drugs, dioxin, radioactive isotopes, or “acutely toxic anti-cholinesterase chemicals” that could wreak havoc with their minds and bodies.
Following a number of news stories, a few protests, and a lawsuit (which failed due to Pennsylvania’s restrictive statute of limitations), the Holmesburg Survivors (as they called themselves) drifted off and resigned themselves to America’s collective indifference to crimes committed against its black citizens. I continued to lecture on the subject at colleges and medical schools such as Brown, Princeton, Penn State, and Washington University in St. Louis. I would often bring a former inmate test subject, Edward “Yusef” Anthony, with me to these events. Yusef’s participation in a variety of medical studies and the harrowing repercussions he suffered were so chilling that I eventually wrote a book about his prison ordeal called Sentenced to Science.
Yusef’s grim experience encapsulated the corruption of the medical and criminal justice systems at the time. Picked up by police as a 20-year-old for selling a small amount of marijuana, he’d spend his time in jail as a human guinea pig testing a wide array of experimental drugs that were of interest to Kligman, the pharmaceutical companies, and the military. For Yusef and hundreds of young black men like him the message was clear—during the 1950s, ’60s, and ’70s, you could be “sentenced to science” as well as prison in Philadelphia.
For years, Kligman and the University of Pennsylvania insisted that they had done nothing wrong. They insisted that they had comported themselves ethically, or at least as most researchers and research universities did during the post-war years. So, in their own minds, there was nothing to apologize for. In fact, Penn even doubled down and continued to honor Kligman with “professorships,” “lectureships,” and other honors long after he had died and his reputation was tarnished. Philadelphia’s 250-year-old College of Physicians, the oldest medical society in the nation, even had the gall to honor Kligman with a Lifetime Achievement Award and a banquet (which was disrupted by protesting Temple University students and former Holmesburg prisoners).
Today, the tide is finally showing signs of turning. In late 2019, just prior to the COVID pandemic, Adrianne Jones-Alston, the 56-year-old daughter of one of the first Holmesburg test subjects to voice opposition to the prison experiments, decided to follow in her father’s footsteps. She started speaking out, writing articles for the Philadelphia Inquirer, Merion West, and other publications letting her readers know what had occurred long ago in the city’s prison system. She described her father’s dramatic changes after he returned from imprisonment, and how the prison experiments disrupted a once loving home. She denounced the university for continuing to honor Kligman and reap the benefits of discoveries obtained at the expense of black prisoners. “Penn has to look at the reality of the fact of the person that they’re supporting,” Jones-Alston told the Daily Pennsylvanian in 2021. “To me, he was a very intelligent and well-versed doctor. He created a great product. He did something good that had a powerful impact on society down to this day. But people were harmed.”
In late 2020, Dr. Jules Lipoff became the first Penn Med School faculty member to criticize Kligman and his own dermatology department with articles in JAMA and the Philadelphia Inquirer. Penn students and faculty began to organize, hold vigils and marches, and publish op-eds criticizing the university for its years of callous indifference. All of this was occurring against the backdrop of the Black Lives Matter protests that followed the murders of George Floyd, Breonna Taylor, and the other high-profile crimes against black Americans.
The house of medicine must ask itself if, given his practices, famous Penn dermatologist and Retin-A inventor Albert Kligman should still be used as an exemplar of research and leadership.
— Jules Lipoff, MD (@juleslipoff) November 25, 2020
Proud to write this in @JAMADerm with @AdeAdamson #dermtwitterhttps://t.co/KXRbzdewol pic.twitter.com/gE5XptlJjg
Fearful of being swept up in a social and racial tsunami, the University of Pennsylvania finally issued an apology. In August 2021, the Dean of the Perelman School of Medicine conceded that it was time “to re-examine how we recognize Dr. Kligman’s legacy.” Yes, he had made “groundbreaking contributions to the field of dermatology,” but “some of his work raised serious ethical concerns”:
Penn Medicine acknowledges that the work done by Dr. Kligman was terribly disrespectful of individuals—many of whom were imprisoned Black men—denying them the autonomy and informed consent which the medical community now considers to be foundational underpinnings for conducting ethical research. Legality, of itself, does not excuse these activities, which are not now, and never were, morally acceptable, even if Dr. Kligman and his contemporaries believed them to be.
The Ivy League school’s apology “for the pain Dr. Kligman’s work caused to incarcerated individuals, their families, and our broader community” was a long awaited landmark event.
Over the course of the following year, the Inmate Justice Coalition, led by Michael Coard, a crusading criminal defense lawyer, and Adrianne Jones-Alston, continued to expose the gross violations that had taken place within the city’s prison system. A letter addressed to Mayor Jim Kenney in late September by Coard and Jones-Alston demanded the city finally own up to its sins of omission and apologize for allowing the county jail to become a for-profit, unsupervised training ground for the University of Pennsylvania’s Medical School. A week later, the Kenney administration responded with “a sincere apology to those who were subjected to the inhumane and horrific abuse,” and expressed its regret that “it took far too long to hear these words.” A week later Philadelphia City Council issued its own apology.
Though the apologies from the City and Penn were significant milestones, leaders of the Inmate Justice Coalition say they are not done. They point out that the District Attorney’s Office, the county court system, and the state—both the Governor’s Office and the legislature—neglected their oversight obligations. Other prestigious groups like the College of Physicians also played a role in allowing the local prison system to become the largest human experimentation factory in post-war America. Educational reforms, demands for compensation, and a reassessment of the critical role played by a pharmaceutical industry that enriched itself at the expense of prisoners’ health are now all up for discussion. It is time to pay up.